Agentic AI is already changing the way we live and work. In fact, by 2025, 85% of enterprises plan to implement AI agents into their business operations. From helping people schedule events to answering live customer questions, they are quickly becoming indispensable.
But when it comes to healthcare, the stakes are higher—and so is the opportunity. AI healthcare agents are poised to transform how health systems operate, engage with patients, and deliver care.
What Is Healthcare Agentic AI?
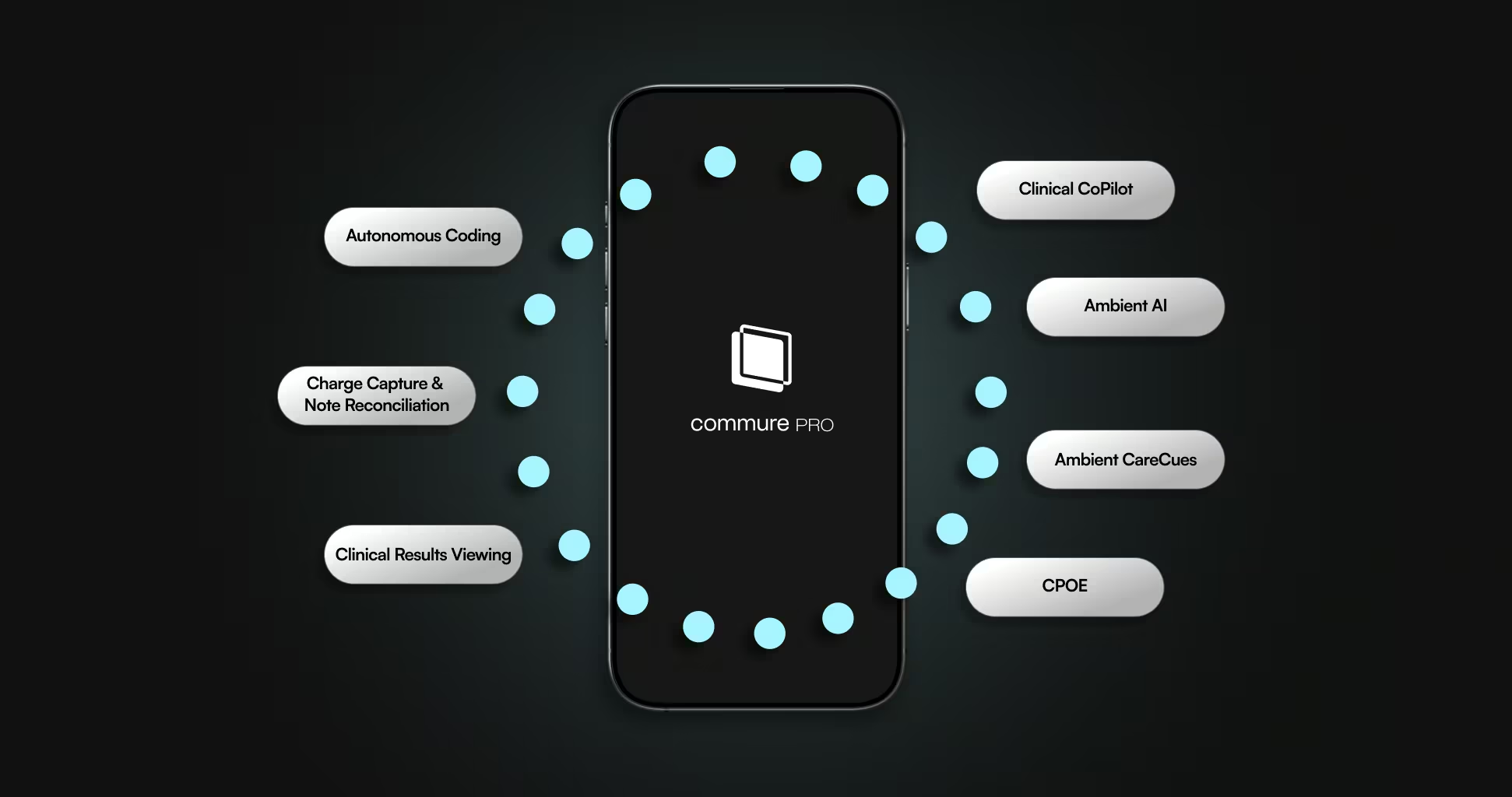
Healthcare Agentic AI refers to intelligent software tools purpose-built to autonomously perform complex tasks across a health system, in coordination with humans and each other. Unlike traditional AI assistants that follow scripts or handle narrow tasks, AI agents operate with greater autonomy, contextual understanding, and adaptability.
These agents are embedded into clinical and operational workflows—not bolted on—enabling them to not only provide information but also take meaningful actions. In healthcare, this means they can proactively streamline patient intake, manage claims, resolve billing issues, generate personalized discharge instructions, coordinate care across departments, and much more.
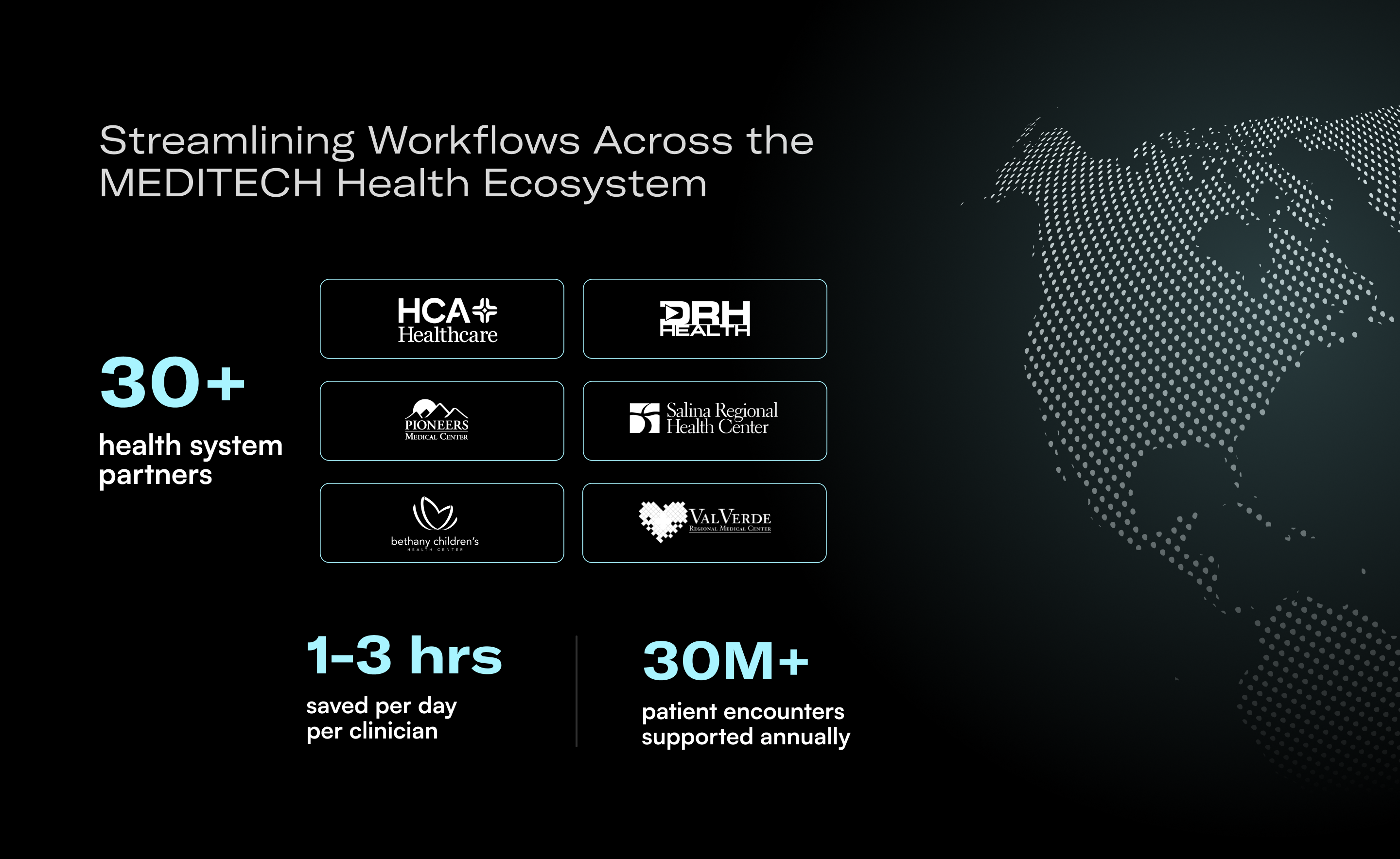
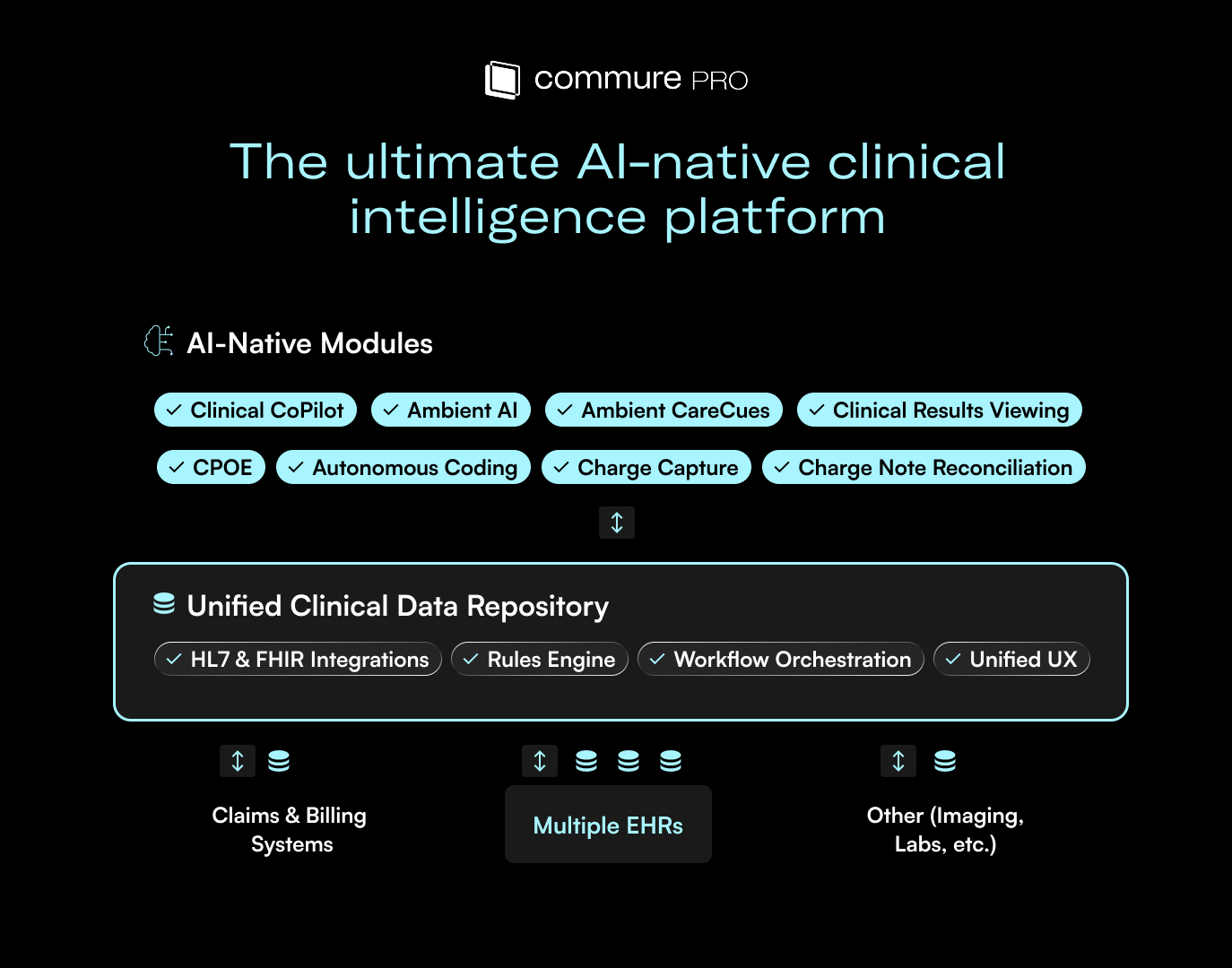
Commure’s Agentic AI platform is designed specifically for the complexities of healthcare, equipping health systems with scalable, secure, and collaborative agents that continuously learn and improve over time.
How Agentic AI Differs from Legacy AI
Legacy healthcare AI systems often rely on rigid rule sets, scripted responses, and limited interoperability. They may work in isolated use cases but quickly break down when faced with the vast scale of modern health systems.
Modern AI healthcare agents, like those powered by Commure, represent a new generation of AI solutions. These agents are proactive, adaptable, and deeply embedded in the tools healthcare teams already use. They can:
- Understand and act on patient data, gaining context from the EHR and documentation from prior visits.
- Integrate with RCM software, documentation tools, EHRs, and other core hospital systems.
- Learn over time, improving responses and automating increasingly complex tasks.
- Operate across departments to coordinate tasks like patient intake, follow-ups, and billing without handoffs or dropped threads.
- Surface relevant information proactively, reducing the time spent searching through EHRs or waiting on callbacks.
- Adapt to changing workflows, policies, and clinical environments without needing reprogramming or retraining from scratch.
This leap from one-off AI tools to collaborative agents will reshape how providers work and care for patients.
Where Agentic AI Has the Greatest Impact in Healthcare
AI agents in healthcare bring tangible value across a wide range of operational and clinical domains:
Patient Access & Engagement
- Proactively reduce no-shows and same-day cancellations.
- Automate appointment scheduling, confirmations, and follow-ups.
- Respond instantly to patient inquiries, improving satisfaction and trust.
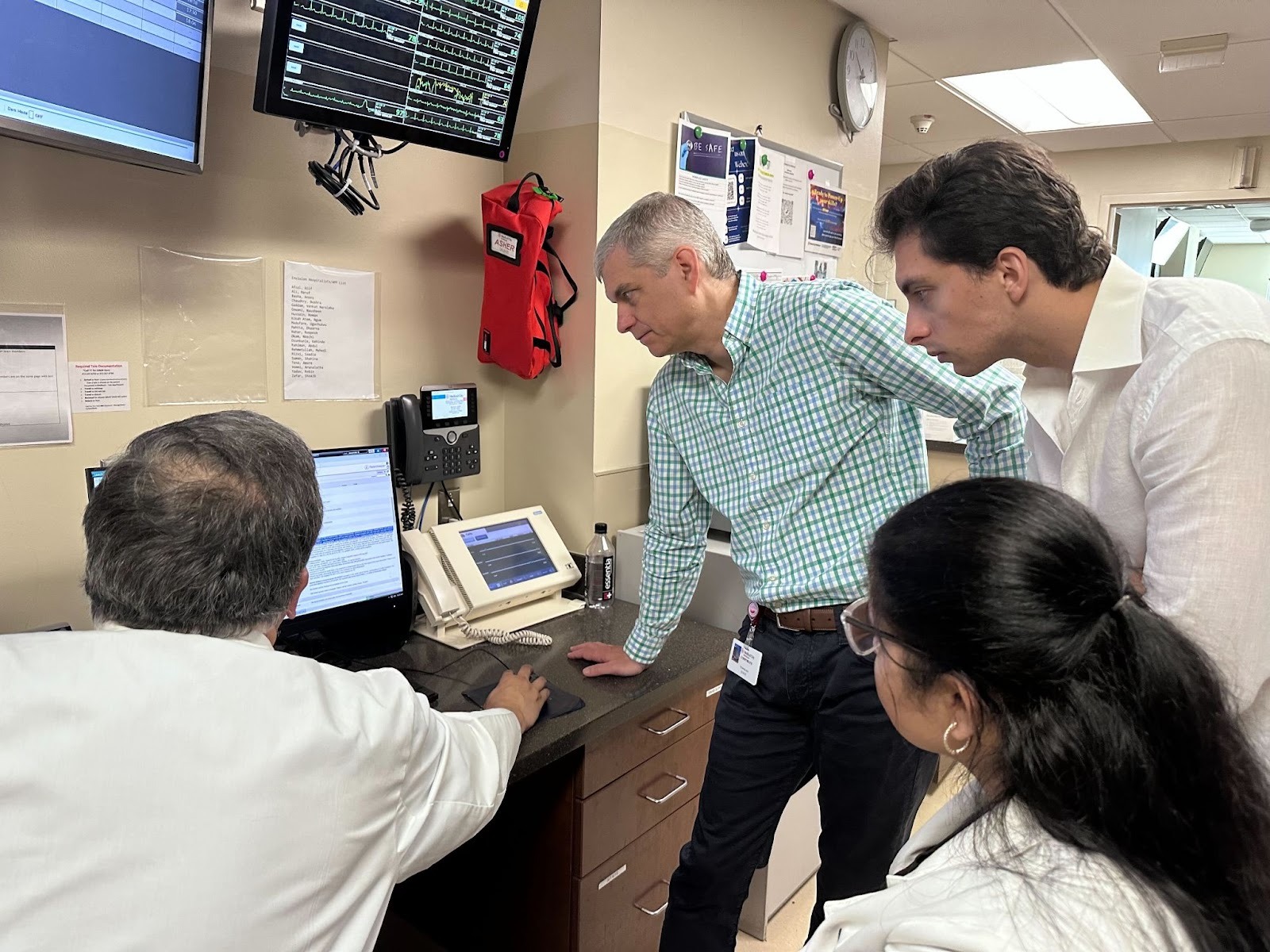
Clinical & Operational Efficiency
- Automate intake, documentation, and routine communication.
- Coordinate care more effectively by connecting staff with real-time data.
- Reduce clinician burnout by taking repetitive work off their plates.
- Improve staff safety by integrating real-time location-aware duress alerts with coordinated incident response protocols
Revenue Cycle & Billing
- Handle billing questions automatically.
- Help patients understand and resolve balances.
- Submit, track, and reconcile insurance claims, identifying inefficiencies and suggesting improvements.
Commure’s Agentic AI offerings are designed to optimize all these areas by deploying tailored solutions across the entire health system.
Choosing the Right AI Partner for Healthcare
As AI adoption accelerates, health systems must be strategic about choosing partners. Not all AI agents are built to handle the complexity of healthcare.
Here’s what to look for:
- Focused on healthcare: Deep domain expertise matters. General agentic AI solutions often miss critical nuances.
- Systemic integration: Agents must work within your existing ecosystem—EHRs, call centers, RCM tools, and beyond.
- Forward-deployed engineering: Successful AI deployments require the right configuration from the start. Look for a partner that provides forward-deployed engineers to configure, optimize, and support your deployment from day one.
- Compliance and trust: HIPAA compliance, data security, and patient privacy must be built into the core of the platform.
Choosing the right partner ensures that your AI strategy evolves with your organization’s needs—not around them.
The Future Is Agentic
AI agents in healthcare are no longer experimental. They’re solving real problems by increasing access to care, reducing burdens on providers, and accelerating revenue.
Commure’s Agentic AI platform represents a new era of healthcare innovation: one where intelligent AI acts as a collaborative teammate across the entire health system.
Ready to see it in action? View the on-demand webianr with Commure for a deep dive into what sets agentic AI apart, key insights on future-proofing healthcare operations, and a live demo showcasing real-world agentic AI applications.






.avif)

.png)