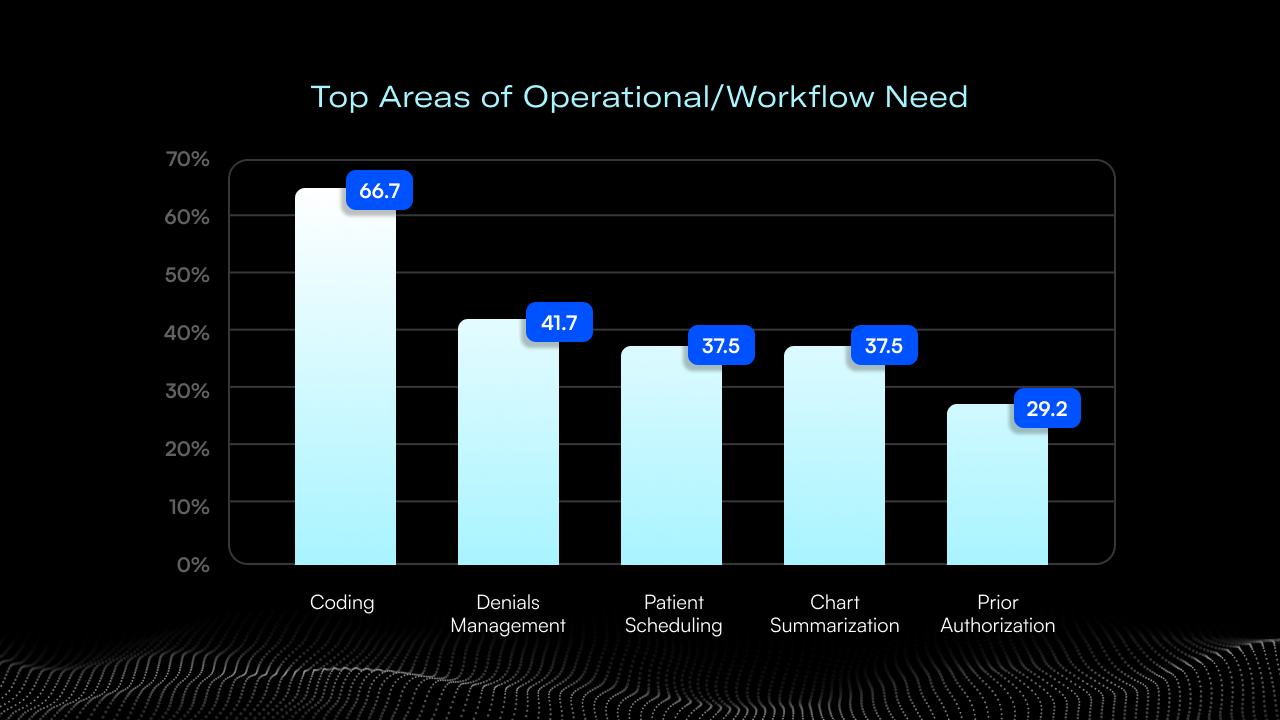
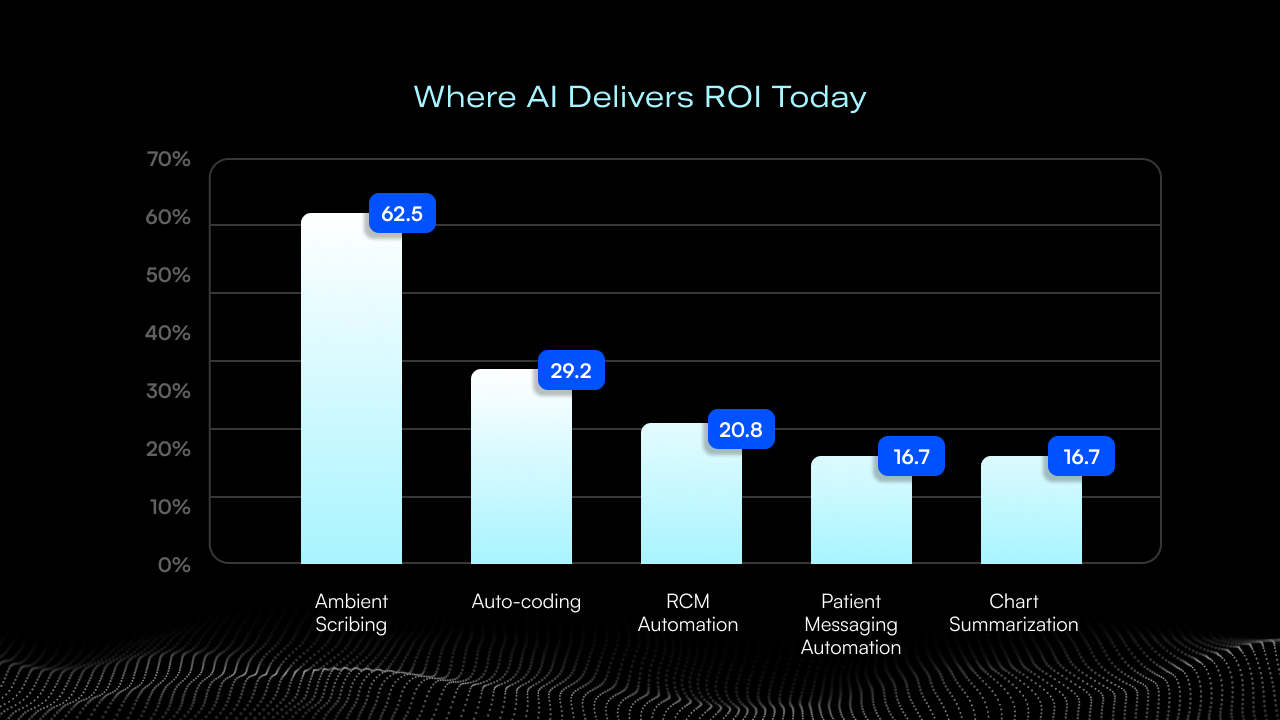
When we surveyed 25 CIOs, CHIOs, CTOs, and digital transformation leaders from major health systems, I expected a wide range of perspectives on AI. What I didn’t expect from our survey of CHIME (The College of Healthcare Information Management Executives) members was how consistent the responses would be. Two numbers in particular stood out: 66.7 percent of these leaders said revenue cycle coding is their most pressing operational gap, and 62.5 percent say ambient scribing is the main place AI is delivering ROI today.
Taken together, the survey results and a follow-up focus group discussion suggest that ambient AI adoption is the tip of the iceberg; an early signal of an industry that is optimistic about AI’s potential to address its most persistent operational challenges, starting with documentation and coding. What I heard from these leaders echoes what I see every week in my work with health systems across the country: AI succeeds when it respects provider and administrative workflows, integrates cleanly, and solves problems that have frustrated clinicians and revenue cycle teams for years.
The Pain Points Are Clear And Persistent
The top operational needs identified by survey respondents were remarkably aligned. Coding led the list by a wide margin at 66.7 percent, followed by denials management (41.7 percent), patient scheduling (37.5 percent), chart summarization (37.5 percent), and prior authorization (29.2 percent).
These pain points aren’t new, and that in itself is telling. Health systems have invested heavily in EHRs, workflow tools, and process redesign. But the underlying issues (operational complexity, information fragmentation, and the administrative weight placed on clinicians) continue to be a challenge. During the focus group discussion, multiple leaders described the burden of keeping disparate tools connected and the frustration clinicians feel when they are forced to jump in and out of systems that don’t talk to each other. As one participant put it, “copy-and-paste is not integration.” And they’re right.
What resonated with me most as a physician was the feeling that many of these challenges aren’t purely technical. Many of these issues are “change management” challenges that involve human and organizational behavior that can be resistant to change.
Where AI Is Working Today
AI is already delivering meaningful value in several key areas. According to the survey, ambient scribing leads the way, with 62.5 percent of leaders reporting positive ROI. Auto-coding (29.2 percent) and revenue cycle automation (20.8 percent) are also gaining traction, with smaller but notable signals in patient messaging automation and chart summarization (16.7 percent each).
None of this surprised me. In our focus group, leader after leader described ambient scribing as the first technology that clinicians find useful and empowering (respondents reported being actively thanked by clinicians for implementing the technology). Some struggled to recruit providers into their early pilots and now have a thousand clinicians using the solution. Others noted that while time-in-chart may not drop as dramatically as vendors promise, the benefits show up elsewhere (more patients seen per day, higher RVUs, more notes closed within 24 hours, and less burnout).
AI doesn’t always generate ROI in the categories we expect, but it consistently reduces cognitive load and gives clinicians the breathing room they’ve needed for years. Clinicians can reinvest that time into catching up on patient messages, reviewing charts, spending more time with patients in the exam room, or relaxing with their families.
The Barriers Ahead: Integration, Trust, and the EHR Black Hole
The survey reinforced an industry reality: 87.5 percent of health systems look to their EHR vendor first when evaluating new technology. At the same time, 70.8 percent prioritize integration ability, and 75 percent prioritize product strength when selecting a vendor.
This dynamic surfaced repeatedly in our focus group. Leaders are open to innovation, with 62.5 percent saying they are willing to adopt best-in-class solutions, but only if those tools integrate seamlessly into existing workflows. Several participants said that once a non-EHR tool is added, it becomes hard to unwind, which makes organizations risk-averse. Others shared frustration that EHR roadmaps for certain vendors often lag behind operational needs, tying their hands and limiting the pace of innovation.
This is not resistance to AI; it is a reminder that technology must fit the ecosystem in which clinicians already live. Trust is built when tools feel native, predictable, and safe. Anything that adds clicks, toggles, or uncertainty will struggle to find adoption, no matter how sophisticated the underlying algorithms are.
Where Leaders Want AI to Go Next
The most energizing part of the focus group was the future leaders described. Many want real-time, context-aware decision support that draws from the conversation in the room, the patient’s history, and clinical guidelines, surfacing insights during the visit, not after. Others are focused on the patient journey, especially the friction points during referrals, care transitions, and post-acute coordination.
Several organizations are investing in enterprise data warehouses or data lakes, hoping to make decades of clinical and financial data accessible for the next generation of AI tools. Leaders are also seeing early wins in operational AI, optimizing the OR schedule, reducing overtime in the ED, and triaging stroke patients more quickly.
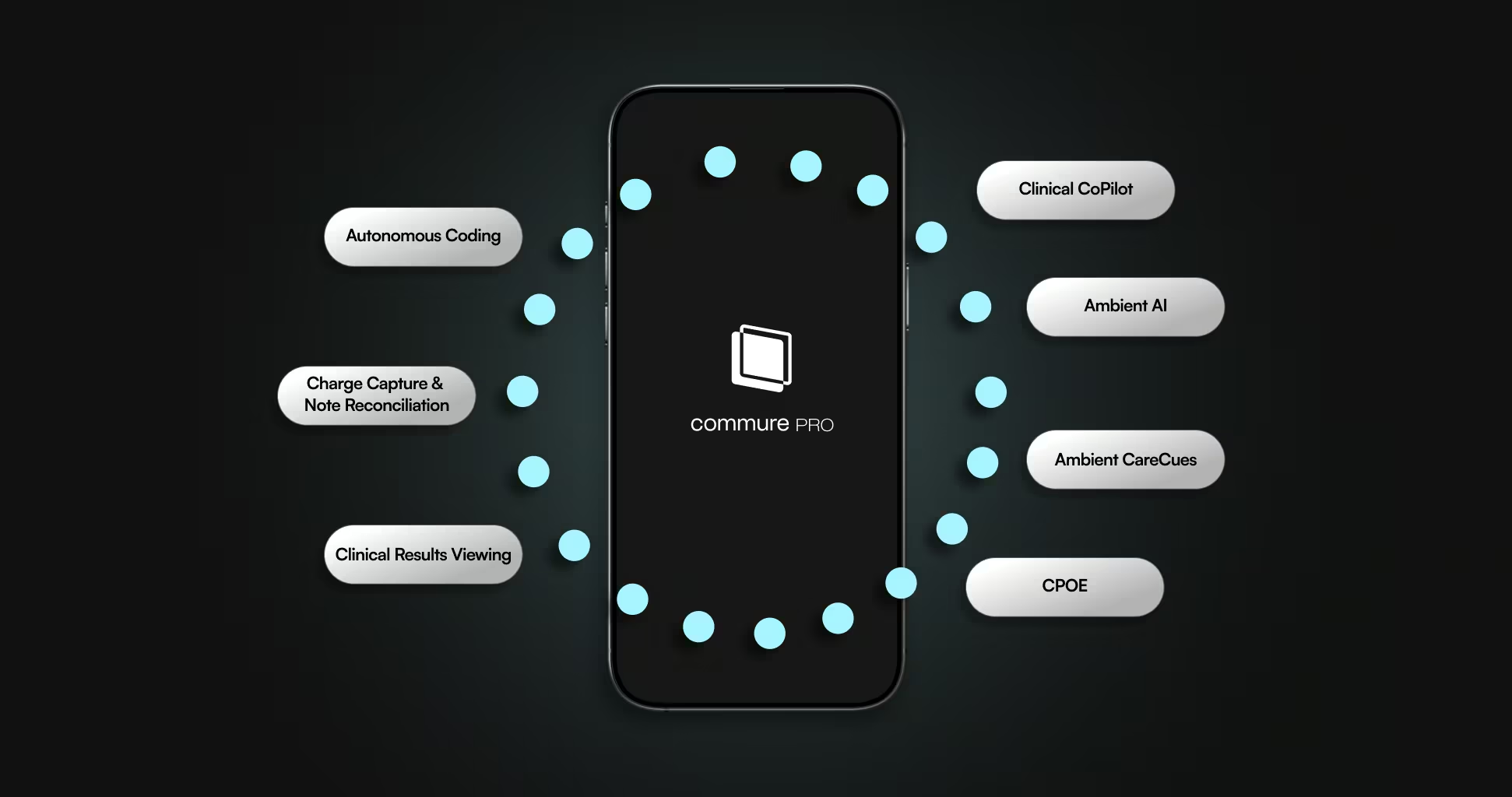
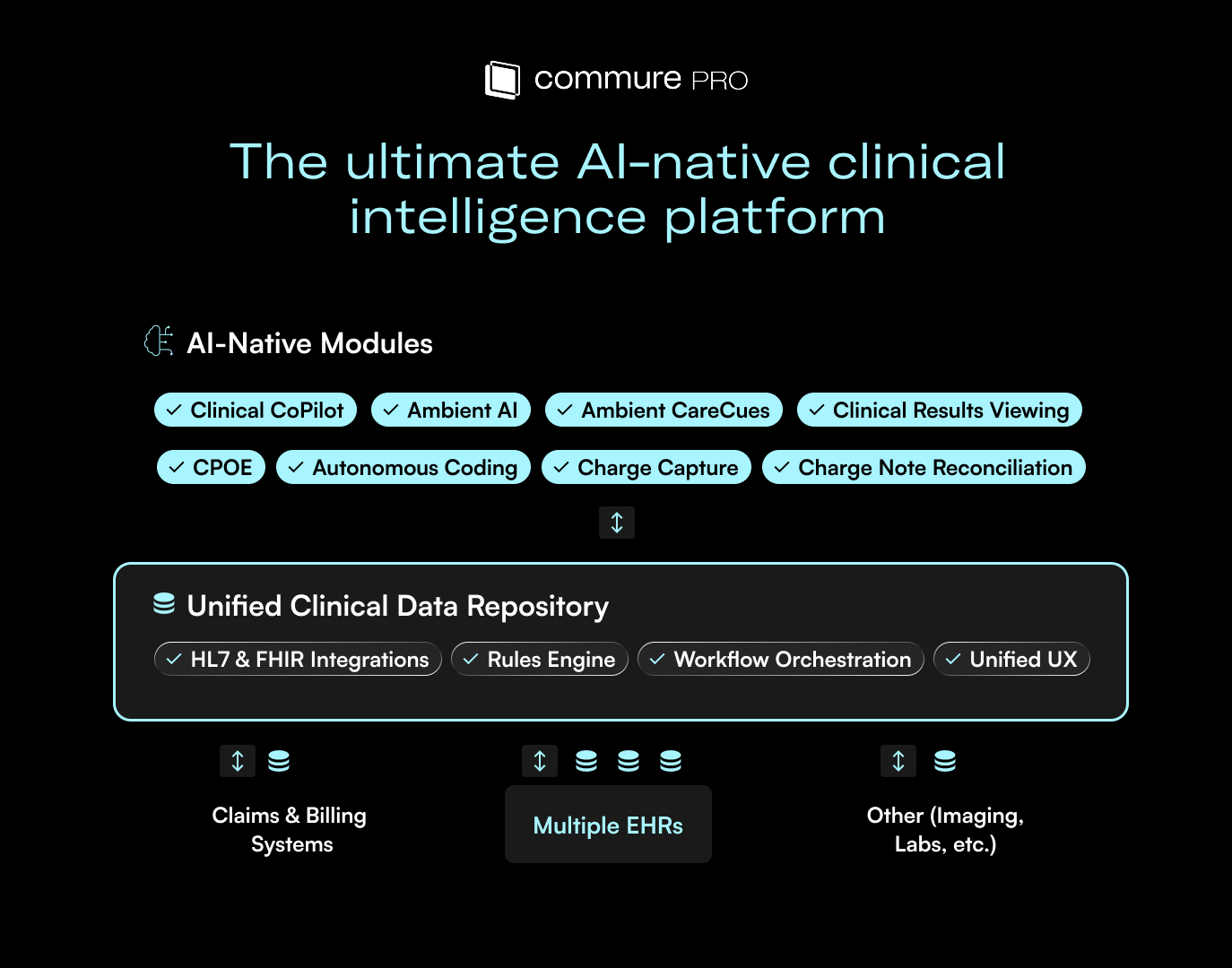
The common thread is that they don’t want isolated tools. They want AI that understands their systems, their patients, and their workflows from end to end. The Commure platform focuses on this end-to-end experience, helping provider organizations deliver higher-quality care at a lower cost.
The Path Forward
The next phase of AI adoption will be focused on execution and the implementation of new technologies into existing service lines. We have seen early wins in ambient scribing and coding automation, and those technologies will be a foundation for what comes next. In order to solve pain points across the entire patient journey, we will need tighter integration, better data foundations, and tools that fit naturally into clinical workflows.
If we stay focused on those fundamentals, AI can reduce friction across the system, strengthen revenue management, and give clinicians time back without adding new layers of complexity. The survey and focus group made one thing clear: health systems are ready to move forward. Our job at Commure is to continue building the technology and the partnerships that make that progress possible.




.avif)

.png)