Artificial intelligence is already reducing documentation burden, streamlining coordination, and improving efficiency across clinical and operational workflows. To explore where AI is delivering real value today and where it needs to go next, Commure hosted Interdisciplinary AI Approaches to Enhance Care Coordination and Improve Outcomes, bringing together leaders from medicine, digital innovation, and applied AI:
- Jean-Luc Neptune, MD (Moderator) – Executive Medical Director, Commure
- Geoffrey Burnham, MD – Hospitalist Medical Director, Medical City Dallas, Envision Healthcare, HCA Healthcare
- Edmondo Robinson, MD – CEO and Founder, Downeast Digital; Former Chief Digital Officer, Moffitt Cancer Center
- Vikash Gupta, PhD – Senior AI and ML Solutions Architect, Amazon Web Services (AWS)
Below are the key insights leaders should focus on as AI adoption accelerates across health systems. You can view the full discussion on demand here.
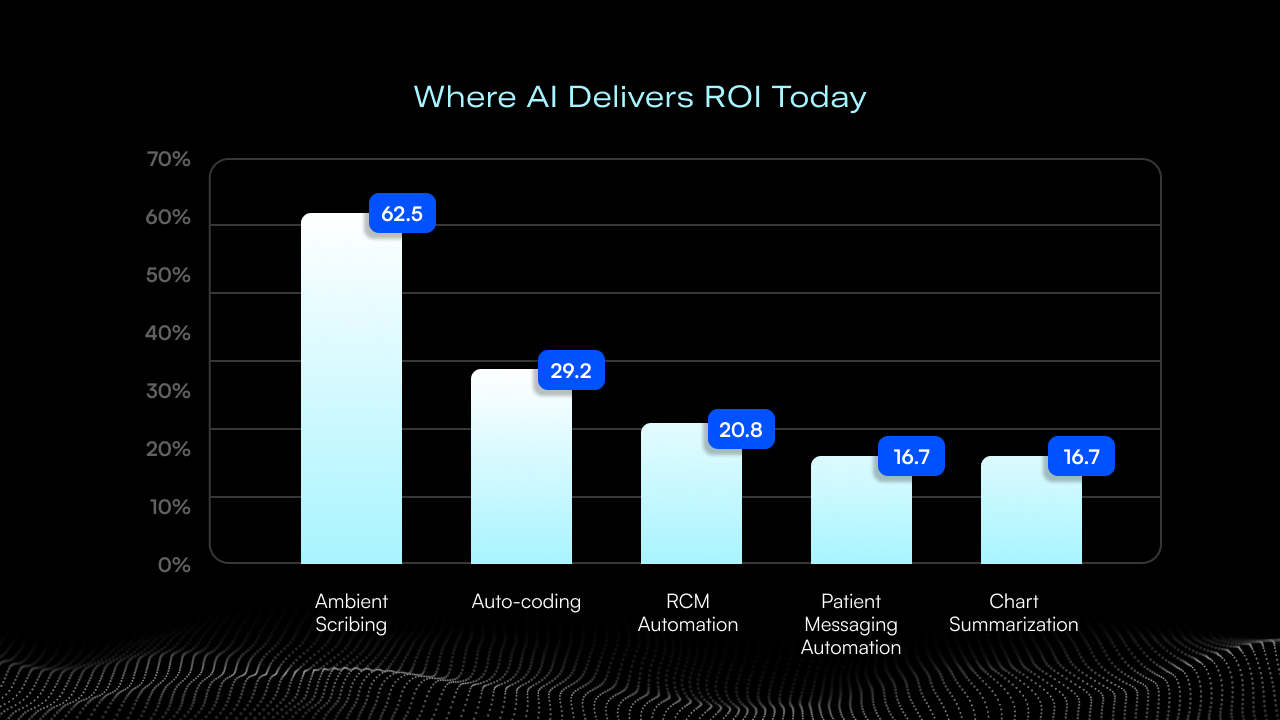
AI in healthcare is real and practical today, especially for documentation and workflow automation.
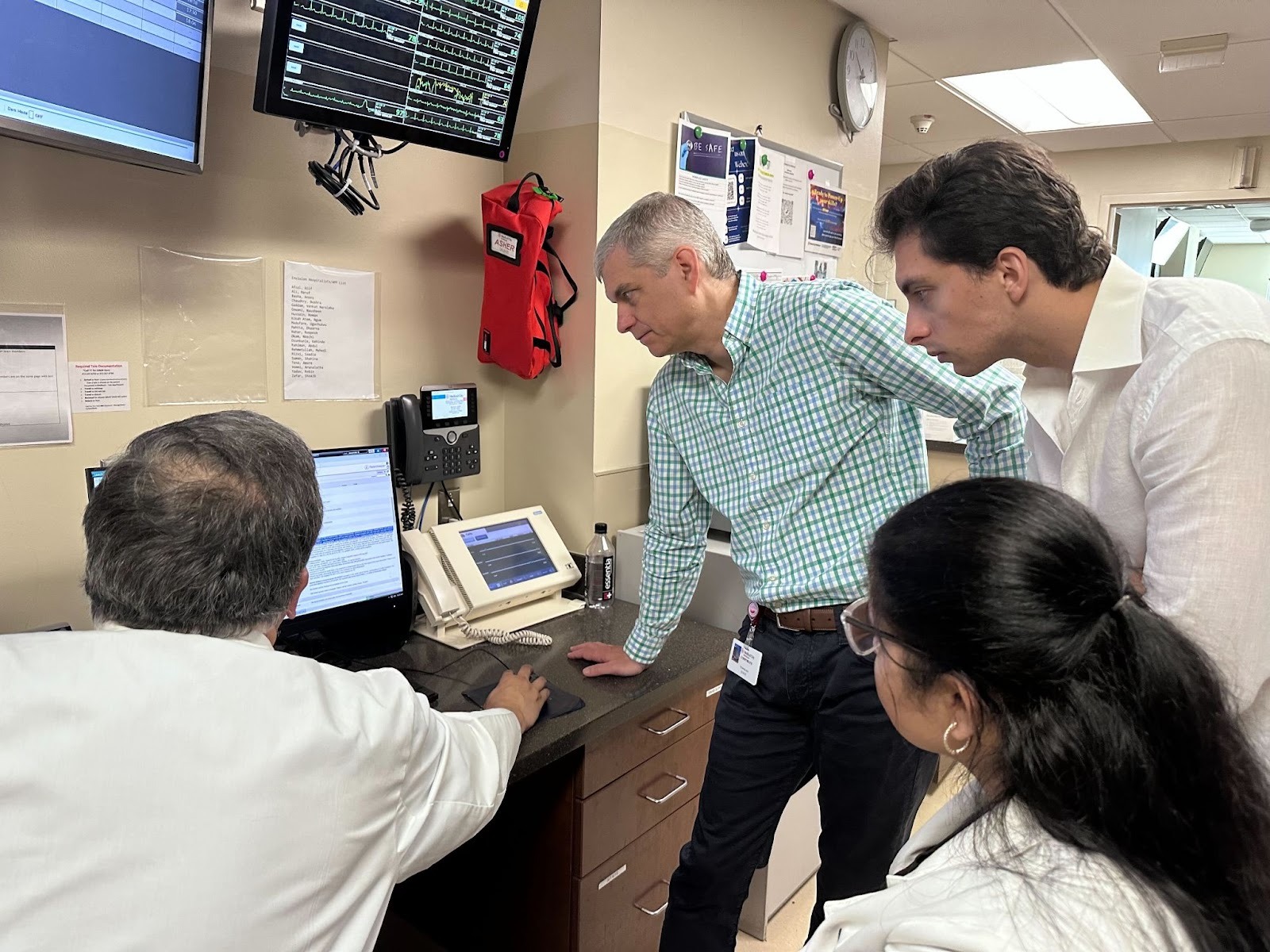
Ambient tools, structured note generation, and task automation are already reducing clinical burden. As Dr. Neptune noted, “Two thirds of a provider’s time is spent in the chart and only one third of that time is actually spent with real patient direct face-to-face interaction.” Redirecting that time back to care teams is one of AI’s most immediate wins.
Take it from Dr. Burnham who’s leveraging Commure Ambient AI at Medical City Dallas, part of HCA Healthcare’s North Texas Division: “Honestly, if I didn’t have it, I’d have a hard time doing my job because of the amount of time it saves and the quality it gives me.”
Trust and transparency in models are essential for clinician adoption.
Ambient AI's success depends on clinicians' understanding what the AI is doing and why. Dr. Burnham explained how his organization builds confidence: "We implemented track changes into our notes where we can actually see what the AI added into the notes. It helps with trust, and it helps with training the model."
While ambient AI reduces documentation burden effectively, precision is critical in healthcare. As Dr. Gupta put it, "Trust is a fragile thing. In the world of AI, if your model is correct 90 percent of the time, that is a great model. In the world of healthcare, a 10 percent error rate is really bad."
A 90% accurate model forces clinicians to spend significant time correcting errors, wasting their time and eroding trust. This underscores why ambient AI solutions must be designed with healthcare-specific accuracy standards and continuous monitoring.
Change management is multi-layered and requires alignment from leadership to frontline staff.
Adoption succeeds when executive sponsorship and grassroots enthusiasm reinforce each other. Dr. Robinson captured the human side of this work: “People are not afraid of change. People are afraid of loss.” Organizations that frame AI as a tool for restoring time and reducing burden rather than replacing jobs see faster buy-in and stronger results.
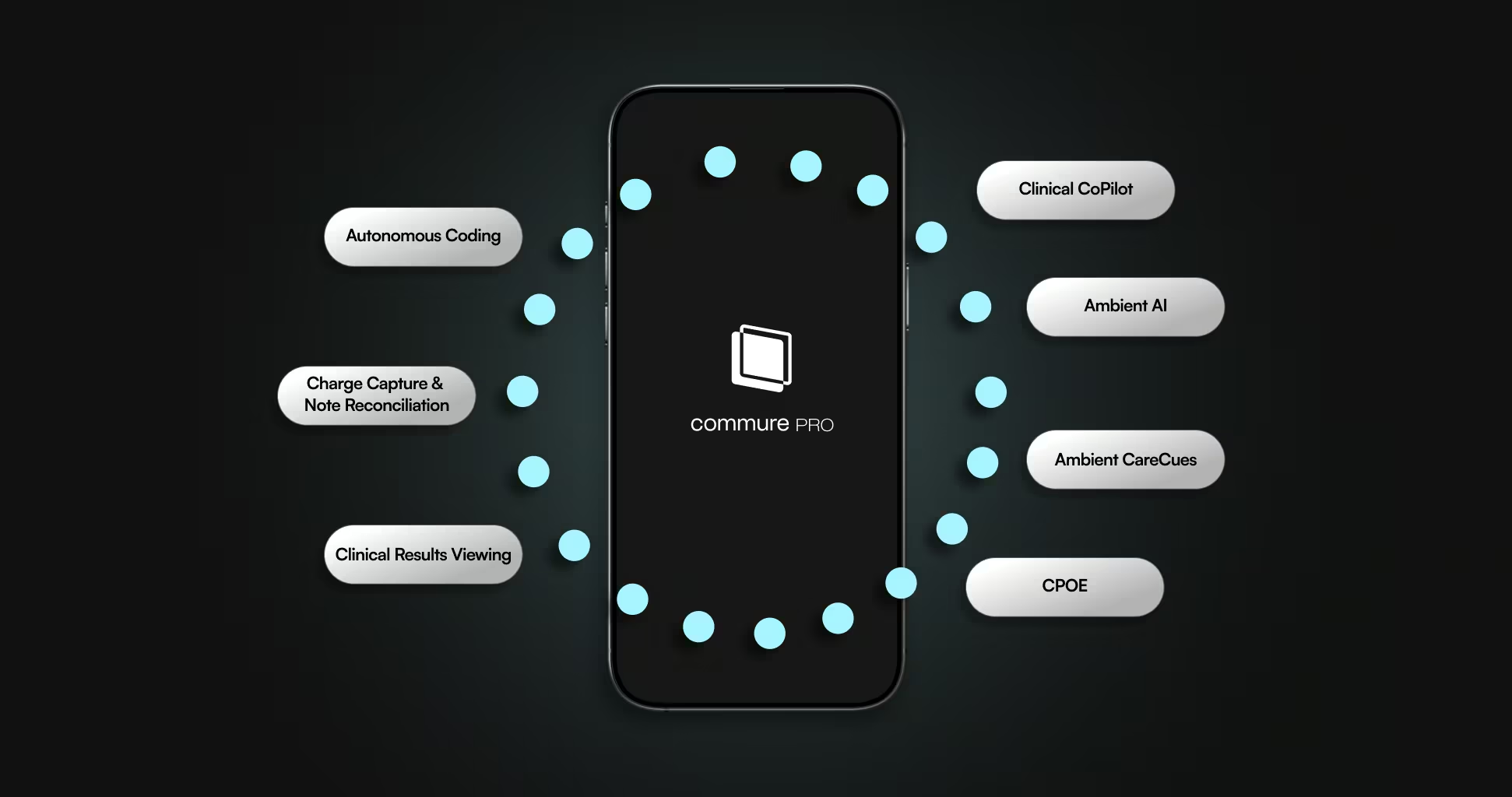
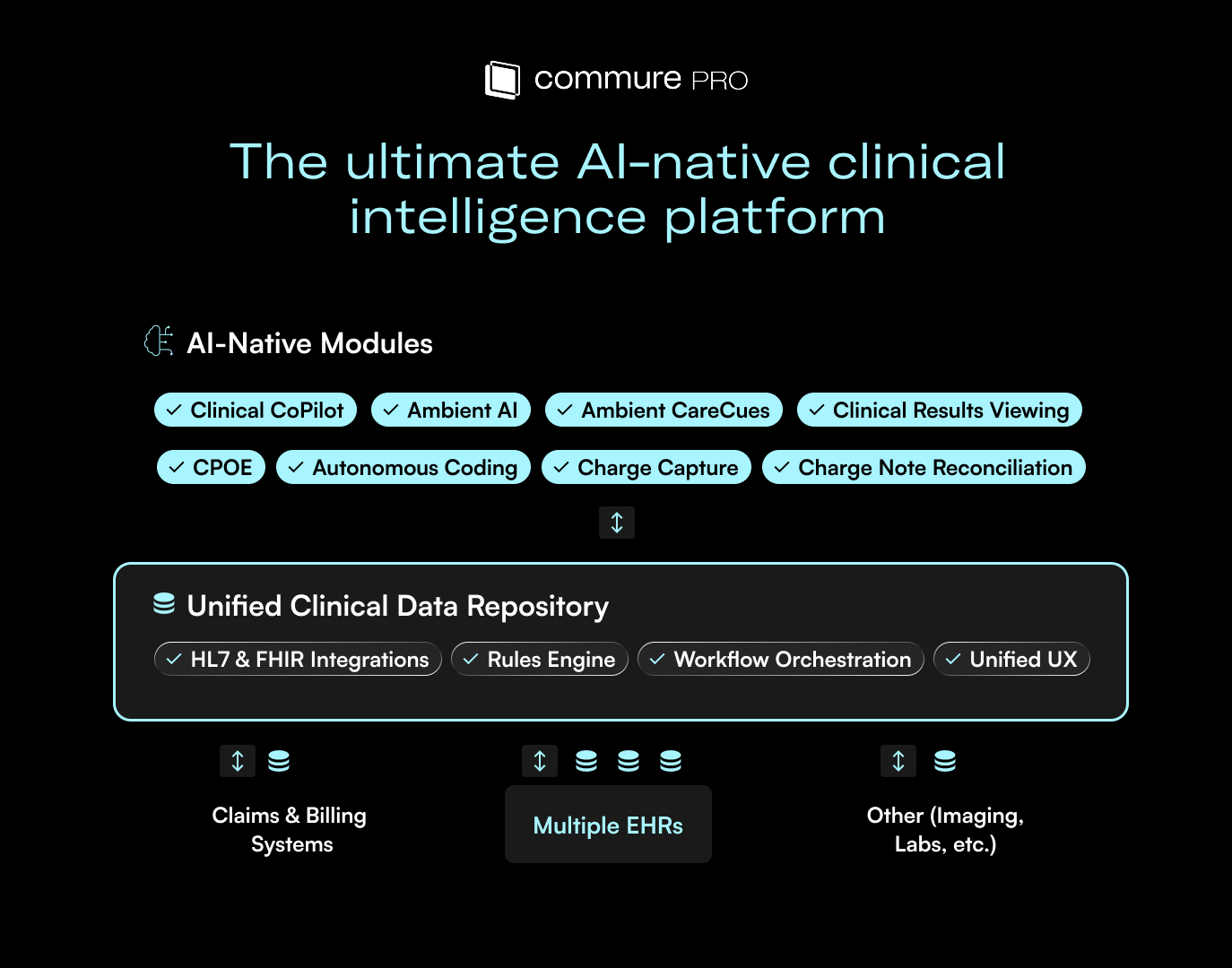
EMR vendors must evolve; open standards and collaboration are critical.
Interdisciplinary AI work depends on interoperability, shared context, and real-time data availability. Closed systems slow innovation and limit value. Dr. Burham shared, “I’ve worked in EMRs where adding one line turns into 13 extra clicks. Multiply that by 20 patients… it’s exhausting.” Future-ready EMR vendors will embrace open frameworks and partner ecosystems that allow AI tools to work across workflows.
Start small, prove value, then scale; land and expand beats big-bang rollouts every time.
The panel stressed the importance of beginning with a targeted use case, measuring lift, and iterating. Continuous measurement keeps adoption honest. As Dr. Gupta said, “Ask the right kind of questions…get to a quantitative measure and that will derive some changes.”
From there, leaders can broaden the footprint of AI across service lines and functions once early wins are clear.
AI should work at the top of its license to amplify, not replace, clinical expertise.
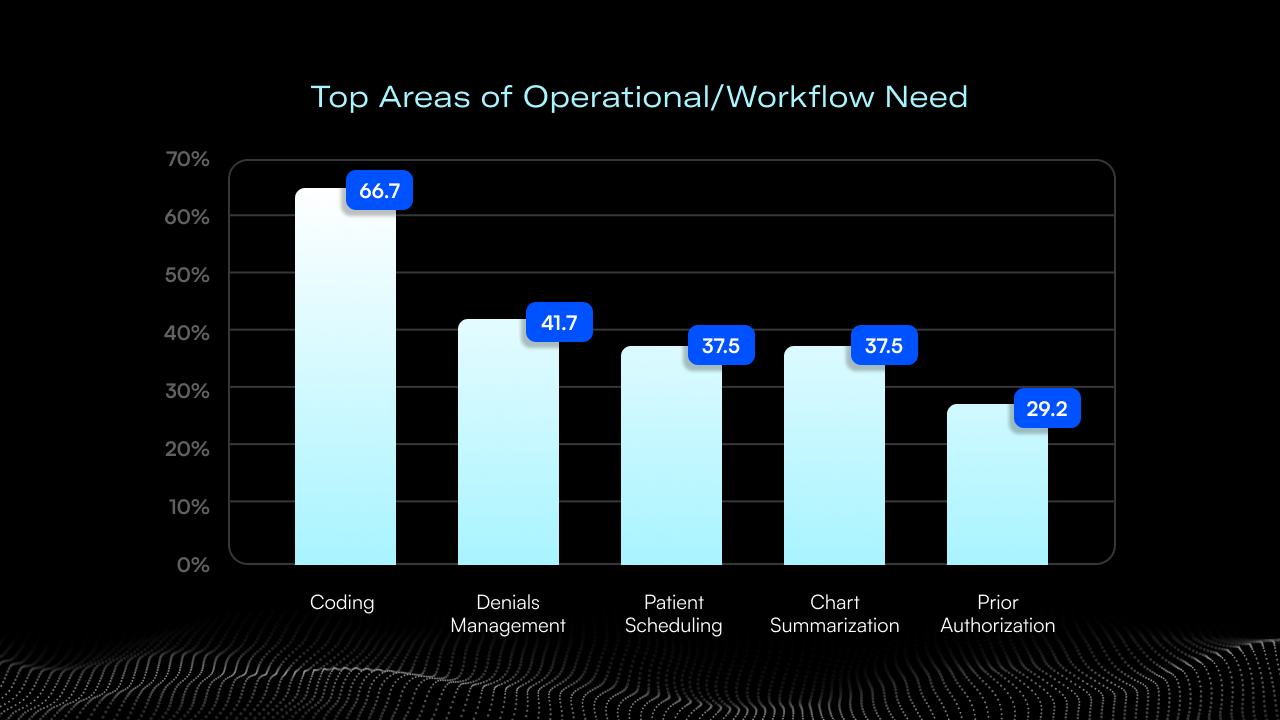
AI’s role is to elevate clinicians by removing administrative friction and enhancing coordination, not to displace judgment. Dr. Neptune pointed to revenue integrity as one example of high-leverage impact: “If you can get your denials from 5% to 2.5%, you’re talking about fundamental impacts on the financial livelihood of the organization.”
Dr. Geoffrey Burnham added, “Clinician buy-in is key. If they see how it makes their lives easier, adoption happens naturally.
Equity and access must remain at the center of AI’s future in healthcare.
Every advancement needs to be evaluated through the lens of patient access, equitable outcomes, and care quality. Responsible leaders build governance that ensures AI closes gaps rather than widens them, particularly for historically underserved populations. Dr. Gupta underscored this sharing, “AI has the potential to bridge that gap, but only if we design for it intentionally.”
AI in healthcare is becoming a foundational capability for documentation, operational efficiency, and care coordination. The leaders who will get the most value are those who focus on trust, transparency, interoperability, and thoughtful change management while keeping equity at the center.
Want to see the full conversation, examples, and perspectives from the panel?
View the Webinar on Demand



.avif)

.png)