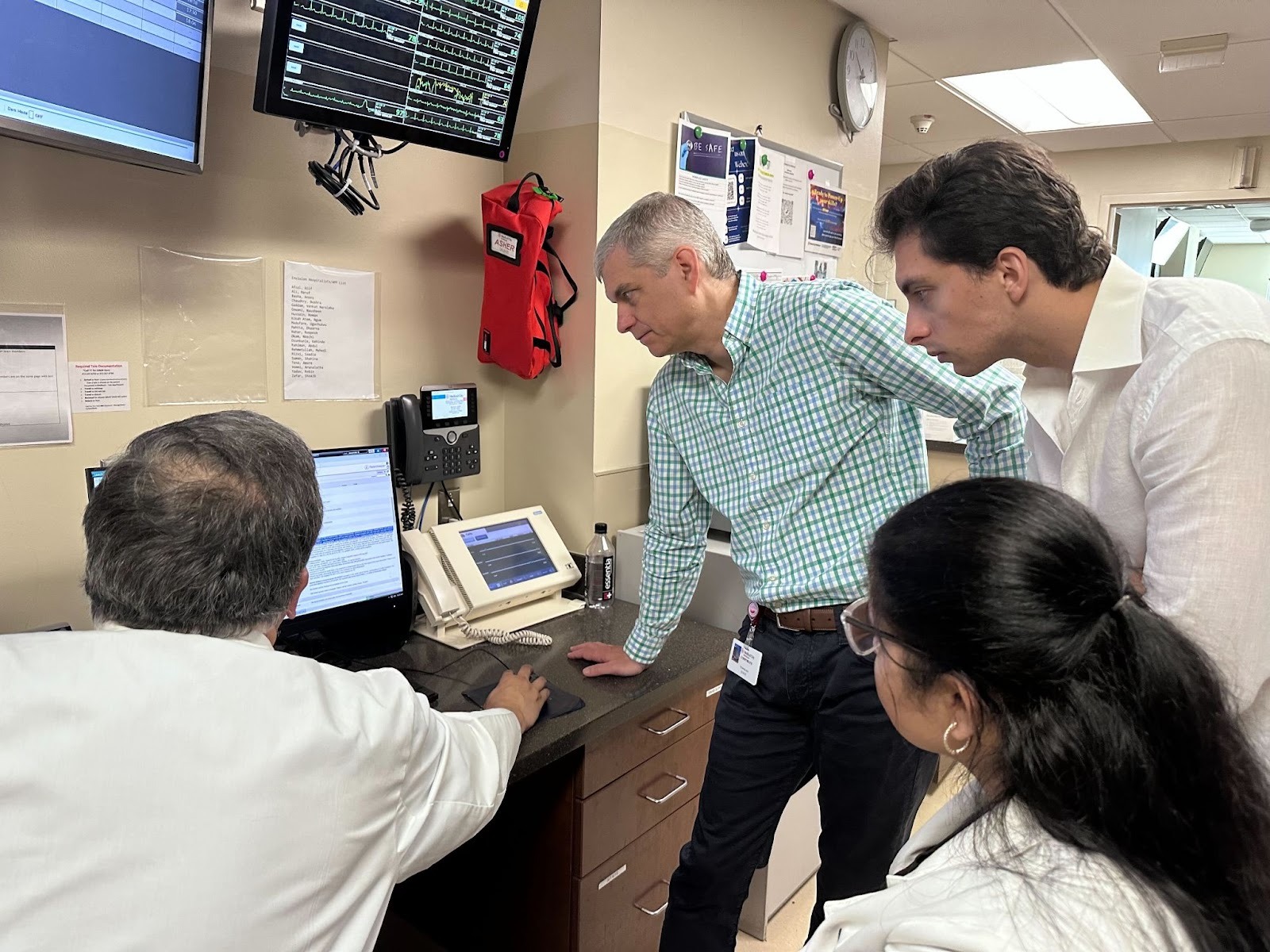
Healthcare innovation usually takes years. At the most recent Commure Nexus, we measured it in hours. Commure brought health system leaders together for a day of discussion on the future of healthcare. During the Forward Deployed Engineering (FDE) Roundtable, executives broke into small groups to surface persistent challenges across the entire revenue cycle, from referral intake bottlenecks to denial backlogs.
Once the discussions wrapped up, Commure’s Forward Deployed Engineering team took those insights and immediately went to work. Over the next four hours, the team built and extended real applications directly from what they heard, combining new builds with purposeful extensions of existing Commure products. Max Krueger, Head of Forward Deployed Engineering at Commure, then took the stage to walk through what the team built and how it mapped back to the challenges raised in the room. Watch Max's full keynote here, or read below for the highlights.
Front Cycle: Reducing Friction Before Care Begins
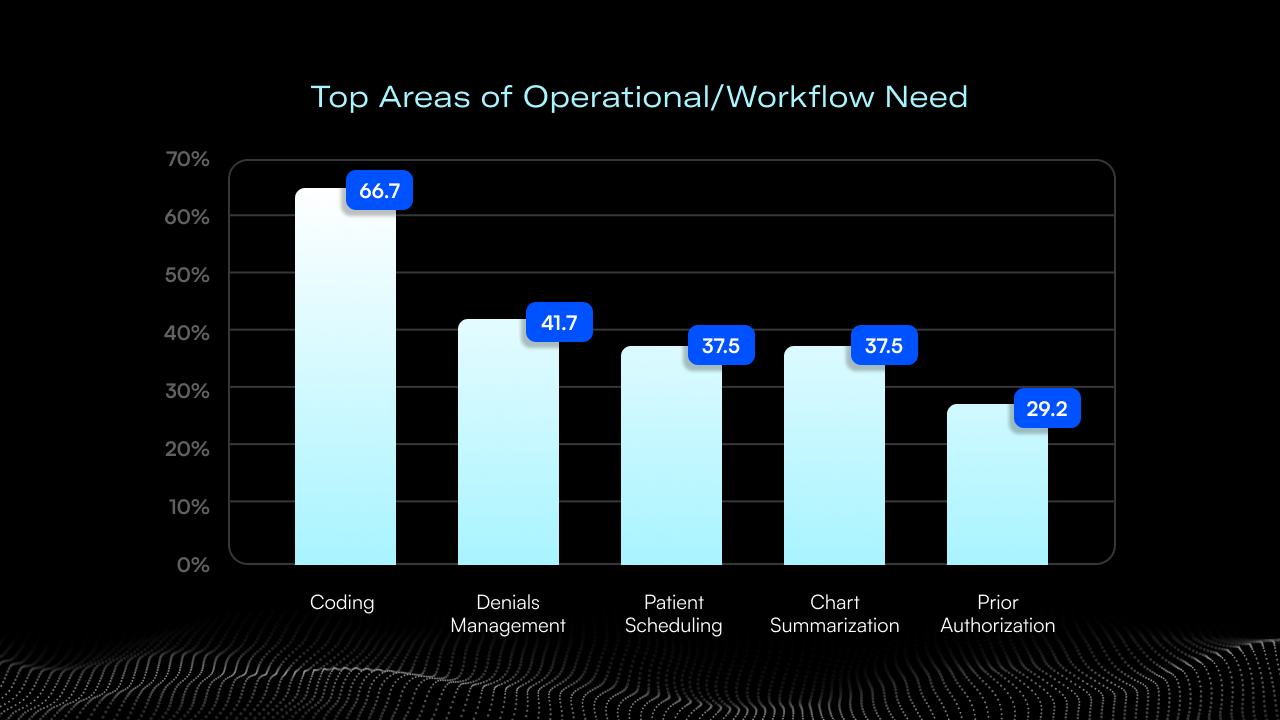
Several of the most consistent pain points surfaced early in the revenue cycle, where manual processes and fragmented information slow both staff and patients down.
One focus area was top of cycle patient admissions and referrals. Health systems currently deploy armies of staff to manually transcribe thousands of faxed PDFs into the EHR. The team deployed AI capable of rapidly ingesting unstructured faxes and converting them into structured, actionable data. Instead of staff manually reviewing long, unstructured files, the system synthesizes key information and makes it available for downstream workflows. What had previously required human interpretation at every step becomes immediately actionable for providers at the point of care.
Another recurring theme was care navigation. Patients often rely on generic tools or external search engines to understand symptoms and next steps. In response, the FDE team configured a health system–specific AI assistant that allows patients to describe concerns in natural language and receive guidance grounded in the organization’s own knowledge bases, care pathways, and clinics. From there, patients can be routed directly to appropriate locations and scheduling workflows, preserving the health system’s clinical and brand context throughout the journey.
Transparency was the third front-cycle priority. Executives emphasized the need for patients to clearly understand their coverage, costs, and next steps. The team extended Commure’s patient engagement platform to present insurance details in patient-friendly language, pre-visit + post-visit summaries, and recommend follow-ups. By delivering this information digitally and proactively, the experience shifts away from paper-heavy processes that are often confusing and easily lost.
Mid Cycle: Bringing Financial Context into the Clinical Workflow
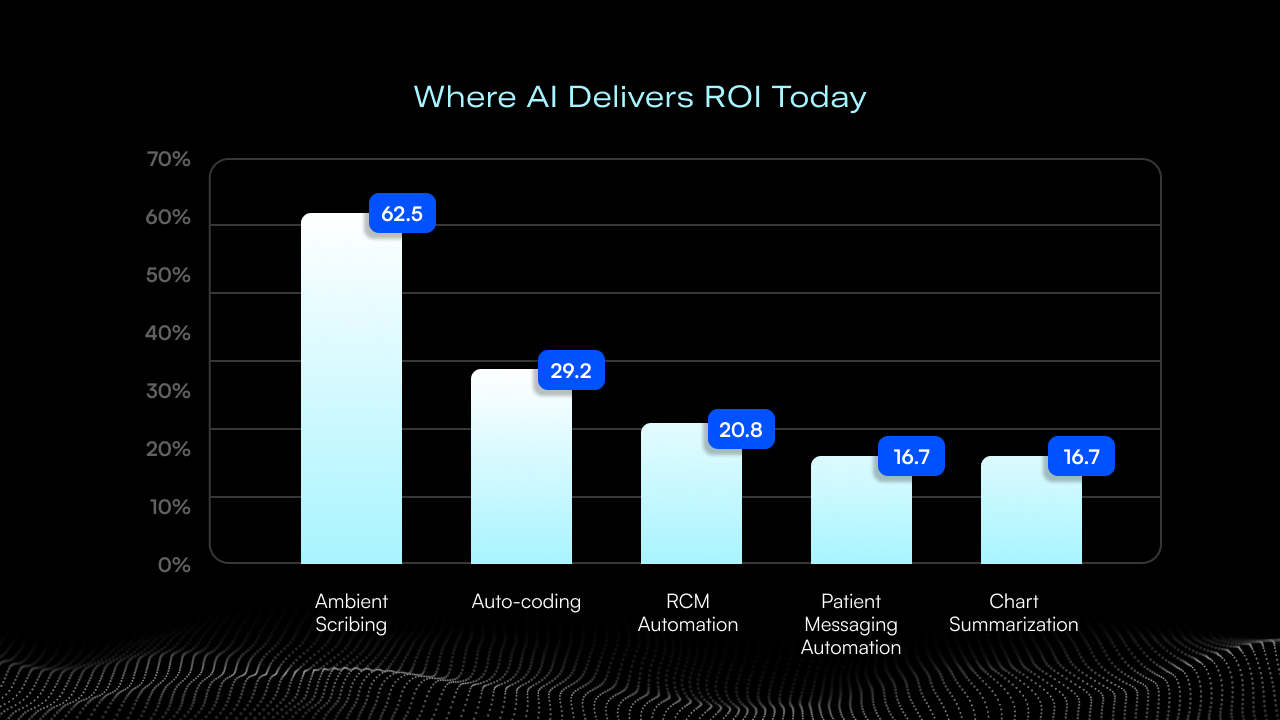
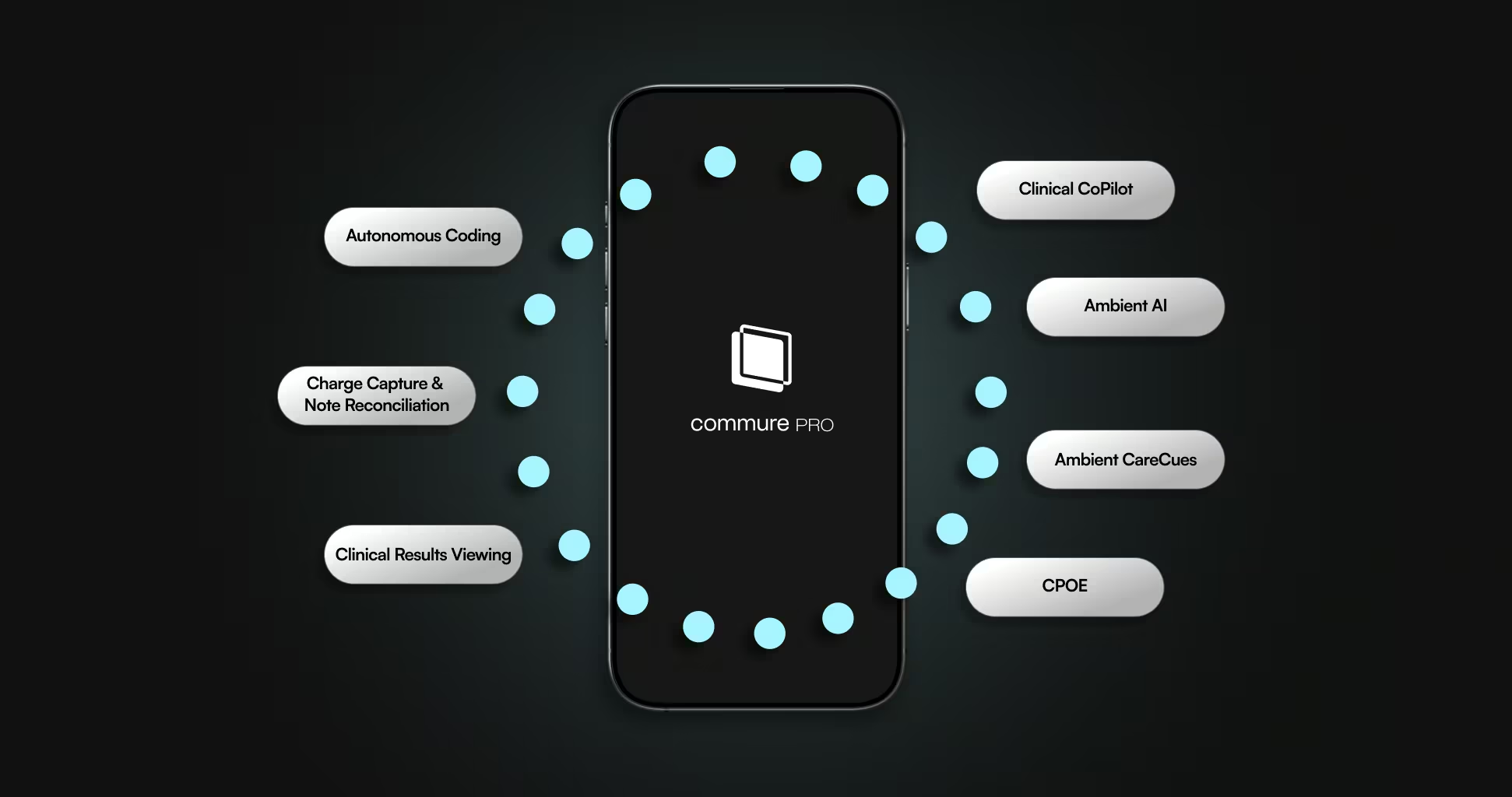
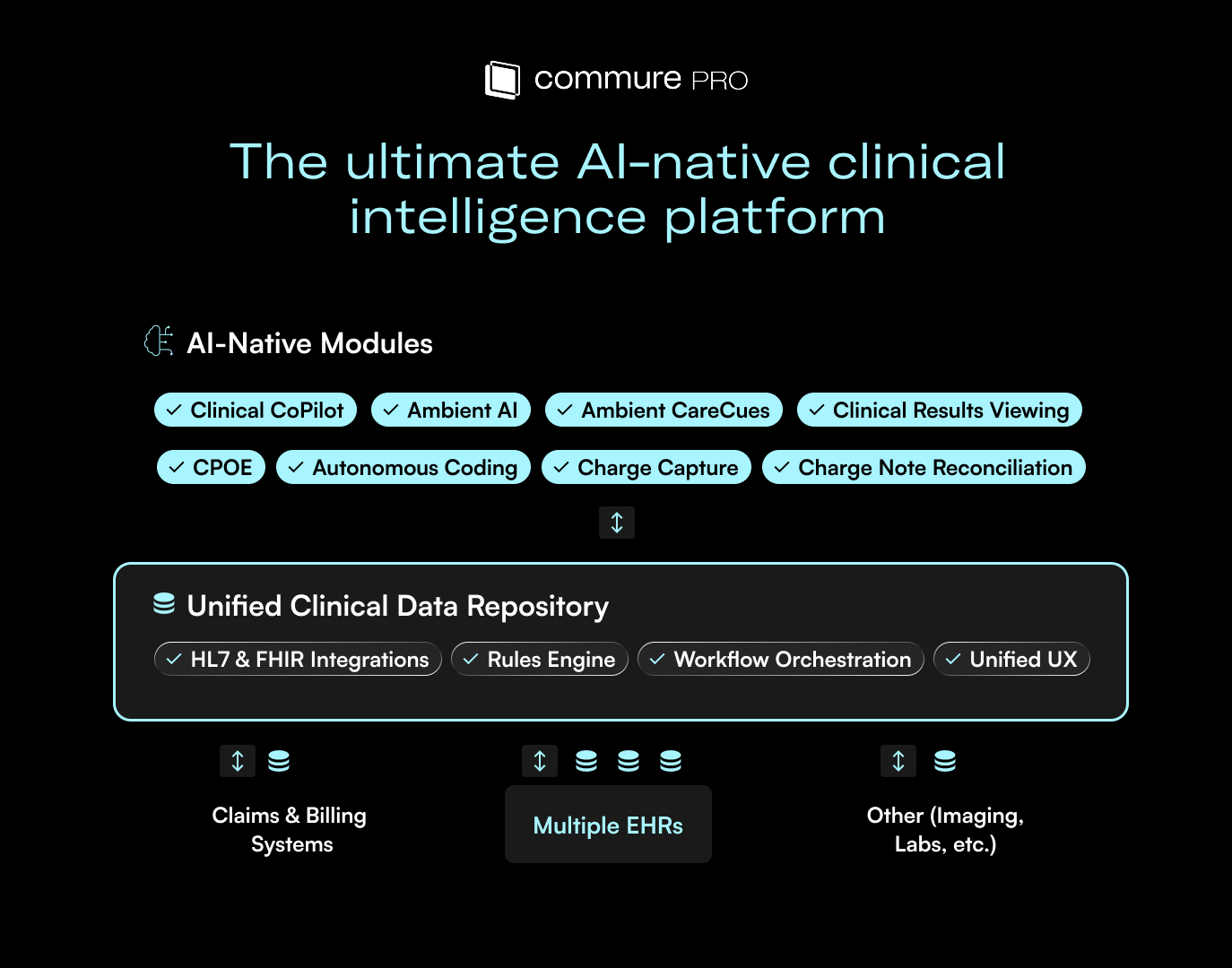
In the middle of the revenue cycle, conversations centered on documentation and decision support during care delivery. While many attendees were already familiar with Commure’s ambient documentation capabilities, the roundtable highlighted an opportunity to surface financial and administrative context alongside clinical insights.
The FDE team extended the ambient platform with live Awareness CareCues that provide real-time visibility into patient profiles, including insurance details and checklist-driven prompts during the encounter. These cues appear directly within the ambient workflow, giving clinicians access to information traditionally buried in disparate EHR tabs or siloed in billing software.
A key use case discussed was helping providers understand where a patient is in their financial journey, such as proximity to deductible thresholds or timing considerations that may affect care planning for patient transparency. By embedding this awareness into the ambient experience, providers gain the same visibility that front desk or billing teams typically have, without disrupting the clinical interaction.
Back Cycle: Scaling Denial Management with Language Models
On the back end of the revenue cycle, denial management emerged as a universally manual and time-intensive process. The FDE team focused on how language models can be used not just to analyze individual denials, but to address them at scale.
The solution analyzed denied claims with full historical context, categorizing based on CARC and RARC codes and prior resolution patterns. Instead of guiding billers through one-off fixes, the system identifies groups of similar claims and enables bulk resubmission across entire categories. This approach shifts denial work away from repetitive, linear processing toward high-impact intervention, allowing smaller teams to resolve large backlogs more efficiently.
What This Demonstrated About the FDE Model
These weren't slide decks or mockups. These were working applications, built in four hours, aimed squarely at the P&L initiatives discussed in the round tables. As Max emphasized, these aren't static tools; they are operational starting points for precision software.
The session highlighted what Forward Deployed Engineering is designed to do: embed engineers alongside customers, work directly from real operational constraints, and move from conversation to working software with speed. Rather than forcing organizations to adapt to static tools, the FDE approach adapts technology to the realities of healthcare delivery.
Want to learn more about Commure’s Forward Deployed Engineering model and how it works with health systems?



.avif)

.png)