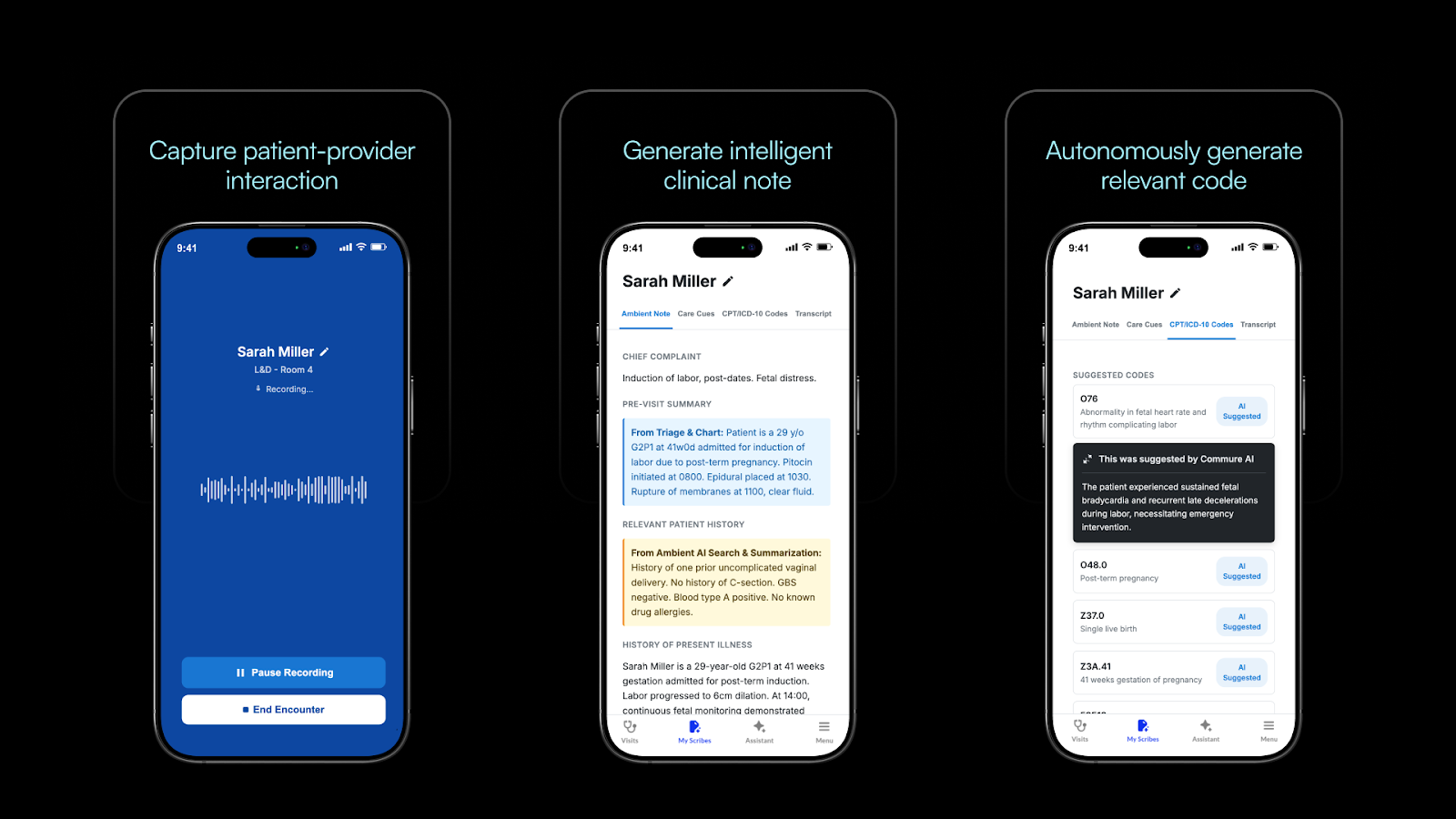
Clinicians didn’t get into medicine to do clerical work, but all too often are occupied by the painful realities of data entry and coding. Commure Autonomous Coding is an AI-powered solution to get clinicians out of the business of coding. It saves clinicians and coders valuable time by automatically generating medical codes from clinical documentation (including CPT codes, ICD-10 diagnoses, and modifiers).
When integrated with the Commure Ambient AI documentation platform, autonomous coding creates an end-to-end experience that transforms how healthcare providers document encounters, submit claims, and optimize revenue capture. Learn more in the video below.
Autonomous Coding: A New Way to Manage Medical Billing
Autonomous Coding represents a fundamental shift from traditional coding practices—breaking the cycle of 'familiar coding' and surfacing secondary diagnoses and specificities often overlooked in manual practice.
How Commure Autonomous Coding Works
Autonomous Coding leverages machine learning and natural language processing to analyze clinical documentation and automatically assigns CPT codes, ICD-10 diagnoses, and without manual intervention. It performs these tasks in seconds, compared with the one-day to six-week cycle common to manual coding submissions and approvals.
Commure’s Autonomous Coding engine leverages multi-layered analysis to ensure accuracy and that every billable aspect of a patient encounter is captured:
- Diagnosis coding: Extracts conditions with specificity that meet MEAT (Monitor, Evaluate, Assess, Treat) criteria from clinical documents.
- Procedure and service coding: Identifies services provided during the visit and follows CPT, AMA, and CMS guidelines to generate codes.
Commure Autonomous Coding stands apart through its reasoning engine, which clearly explains every code it assigns. After codes are generated, providers can review the complete rationale—including medical decision-making logic, risk levels, time calculations, and direct references to supporting clinical documentation. This transparency helps providers understand, validate, and trust automated coding decisions while staying compliant with regulations.
.png)
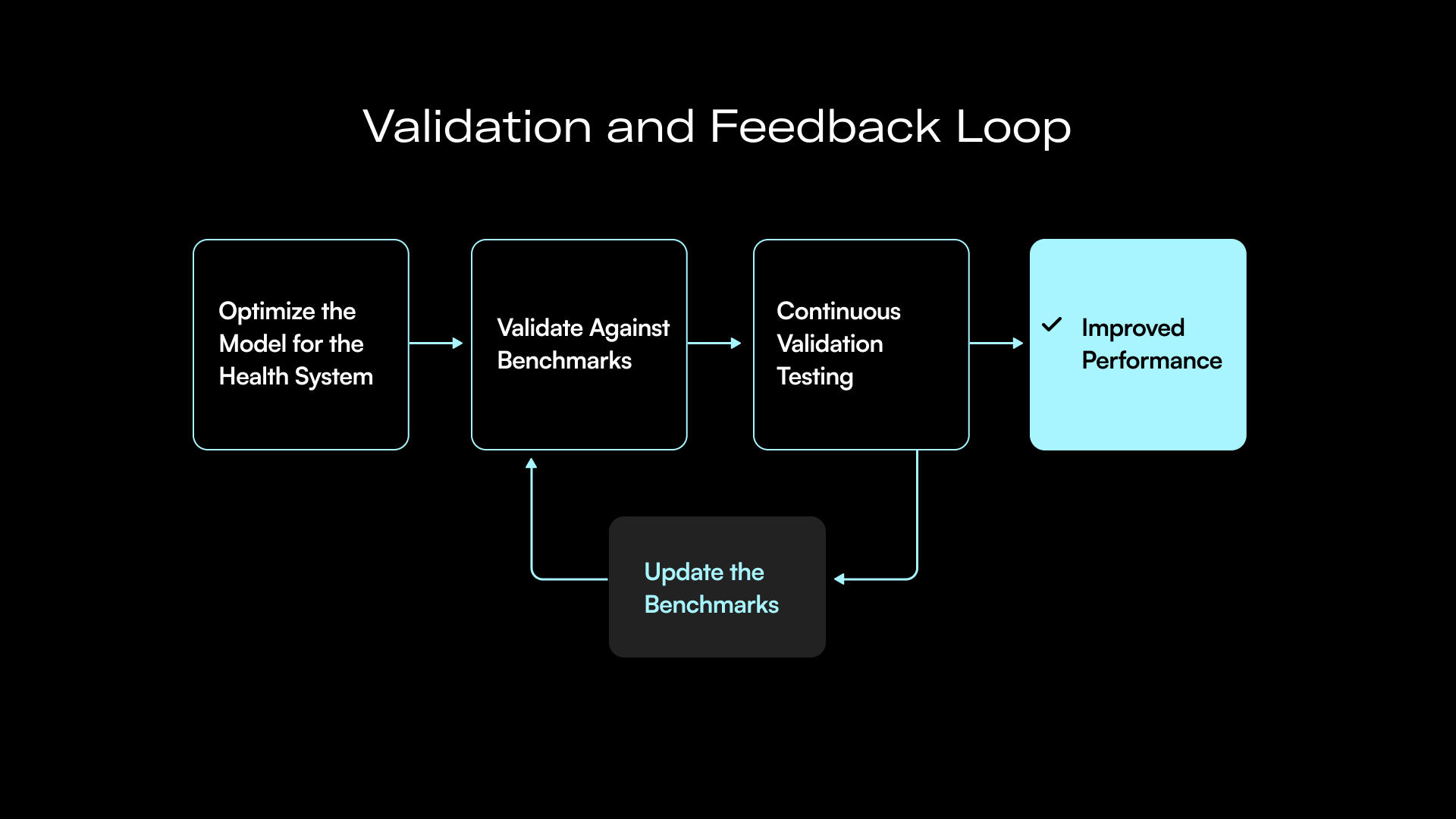
Validating and Continuously Improving the Model
What distinguishes Commure Autonomous Coding is its strict validation and continuous improvement model, which ensures that the model performs well based on client-specific data. This process includes:
- Benchmark Dataset: Before implementation, the Commure team reviews historical billing records to create gold standards”for every type of charge. This ensures that when a charge is generated for a real patient, it is based on the most accurate coding methodology.
- Continuous Testing: Commure conducts validation testing of suggested codes against historical coding data from large health systems. Across almost every customer tested, coding auditors have noticed patterns where the AI model selected more appropriate codes than what human coders had originally assigned.
- Customized Billing Rules: The solution includes health system and network-specific rules and can layer on payor-specific guidelines as they are updated.
- Quarterly and Annual Updates: Coding Guidelines are reviewed annually and quarterly as released, with the option for ad-hoc updates as needed. This ongoing maintenance keeps coding accurate and compliant as requirements change.
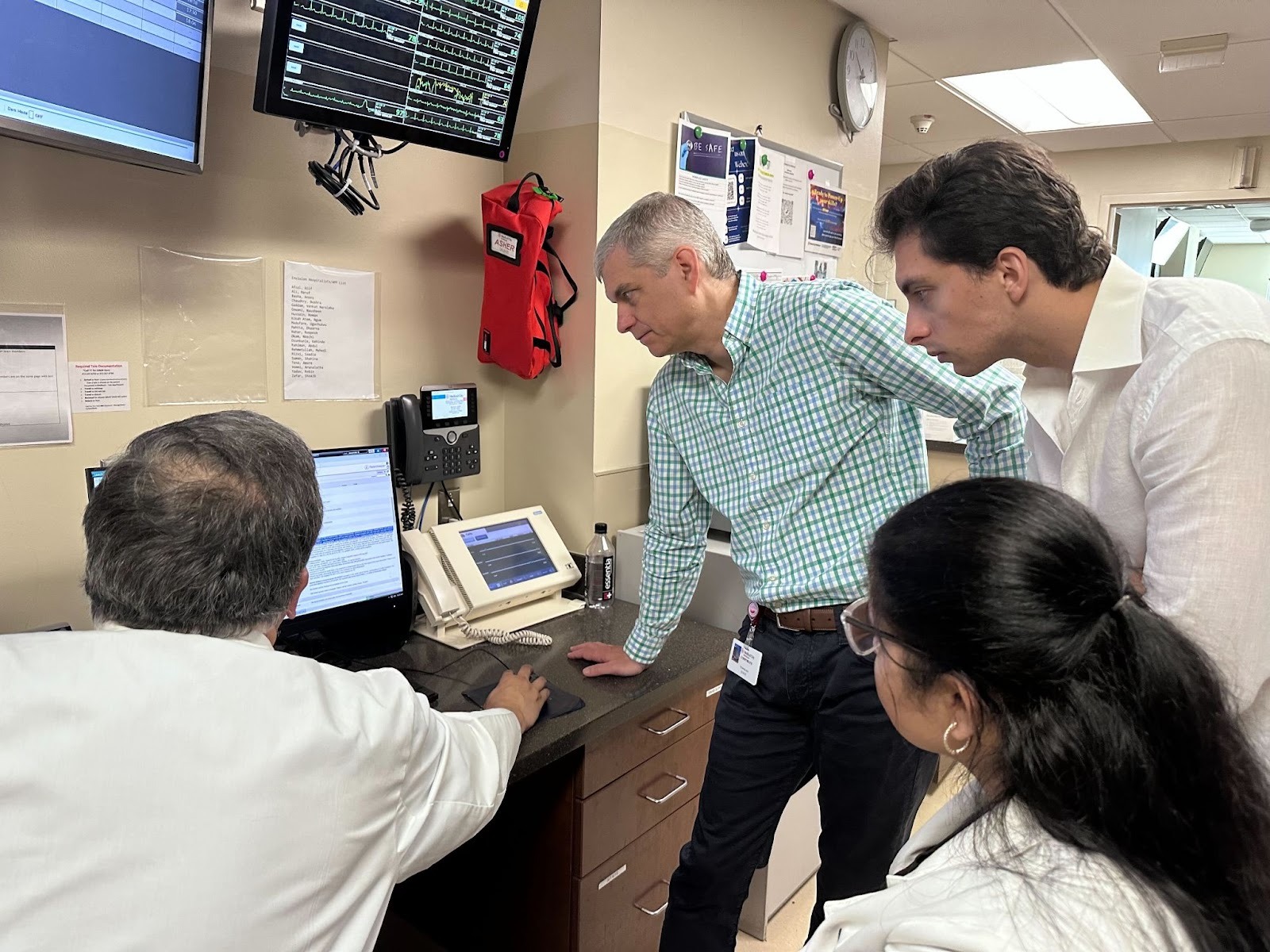
Optimizing Autonomous Coding Deployments with Forward Deployed Engineering
Building an effective autonomous coding workflow demands multidisciplinary expertise and strong integrations across multiple systems. Commure’s approach brings together clinical insight, technical depth, and coding proficiency. A typical Commure Autonomous Coding implementation includes:
- Clinical Expertise: A medical doctor serving as Clinical AI Strategy Lead oversees process strategy and ensures clinical alignment, bridging the gap between AI capabilities and real-world clinical workflows.
- Engineering Leadership: An experienced engineer will lead architecture and development, supported by specialists in E/M automation, ICD-10 logic, product functionality, and quality assurance.
- Coding Proficiency: Certified medical coders (CPC, CPC-I, CBCS) ensure the system adheres to the latest coding guidelines and regulatory requirements.
- Implementation Support: Implementation specialists facilitate smooth deployment and integration with existing systems and offer round the clock support for critical IT issues.
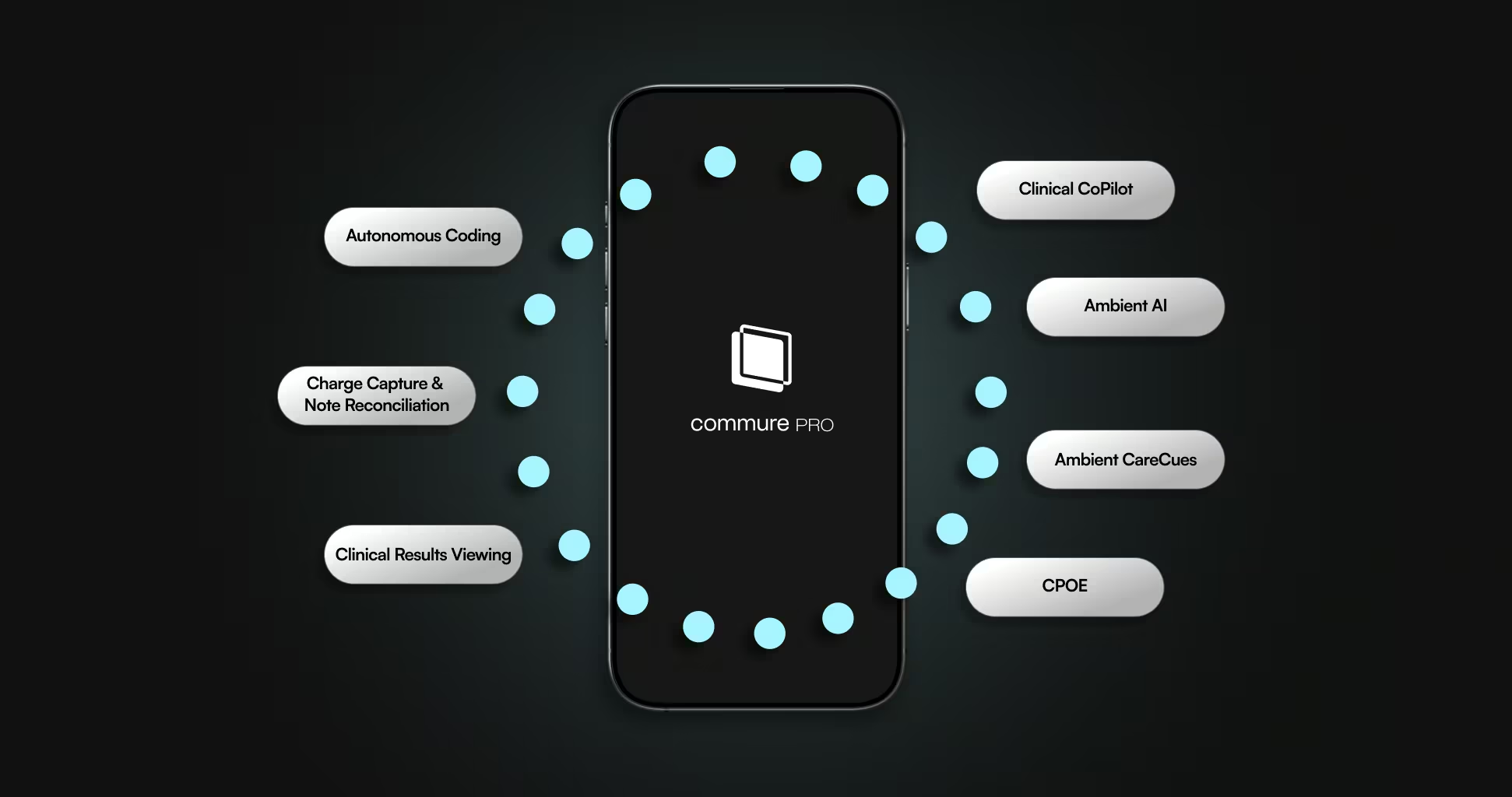
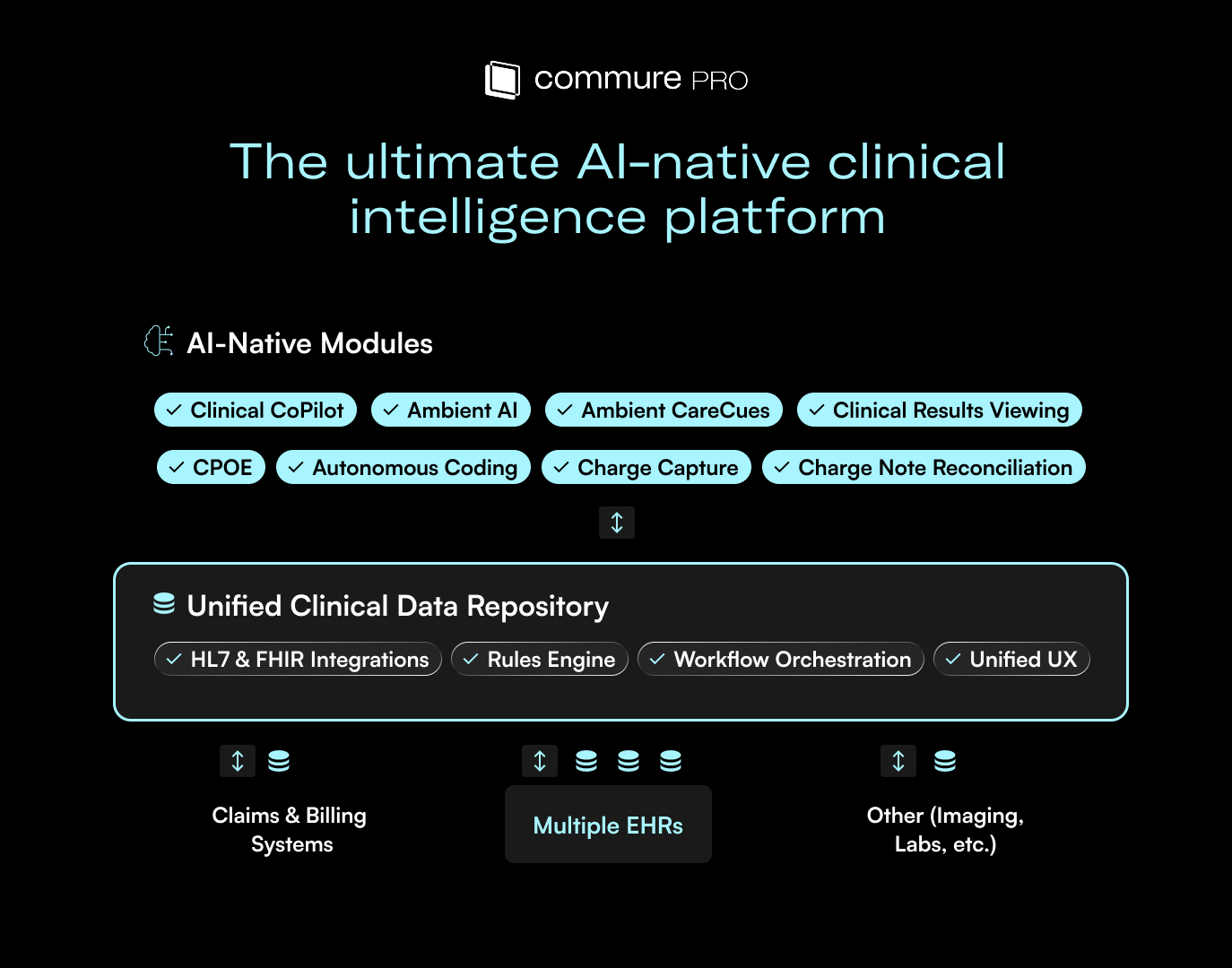
How Autonomous Coding Fits within the End-to-End Journey
Autonomous Coding serves as a pivotal connector within a comprehensive, end-to-end revenue cycle ecosystem that mirrors the full patient experience. When used alongside Commure Ambient AI and its Clinical Documentation Integrity module (aka CareCues) at the point of care, and reinforced by the downstream intelligence built into Commure RCM, it creates a continuous thread from the clinical encounter through to a fully coded, comprehensive claim. This seamless alignment elevates individual efficiency gains into broader, enterprise-wide improvements for patients, clinicians, and operational teams.
A Transformative Technology for Healthcare
Autonomous Coding signifies a crucial turning point in healthcare revenue cycle management, offering exceptional improvements in speed, accuracy, scalability, and cost-effectiveness.
For physicians, this technology reduces administrative loads, allowing more focus on patient care. For coding professionals, it eliminates routine tasks and frees them up for complex, high-value work that utilizes their skills. For revenue cycle managers, it speeds up cash flow, enhances accuracy, and provides scalability without proportional staffing increases.
As the technology evolves and expands, autonomous coding will become a key element of healthcare revenue cycle operations. Interested? Reach out to learn more about Commure Autonomous Coding.

.png)



.avif)

.png)