As artificial intelligence systems grow more capable, the question facing healthcare leaders is not whether to adopt AI, but how to deploy it responsibly. According to Commure CEO Tanay Tandon, effective AI integration in health systems depends on several critical factors: the nature of the task, the role of human oversight, the equity of outcomes, and the degree of collaboration with clinical end users.
“This is a fundamentally new way of interacting with technology,” Tandon explained. “Instead of explicitly programming rules and heuristics, you’re working with systems that have absorbed millions of documents and examples.”
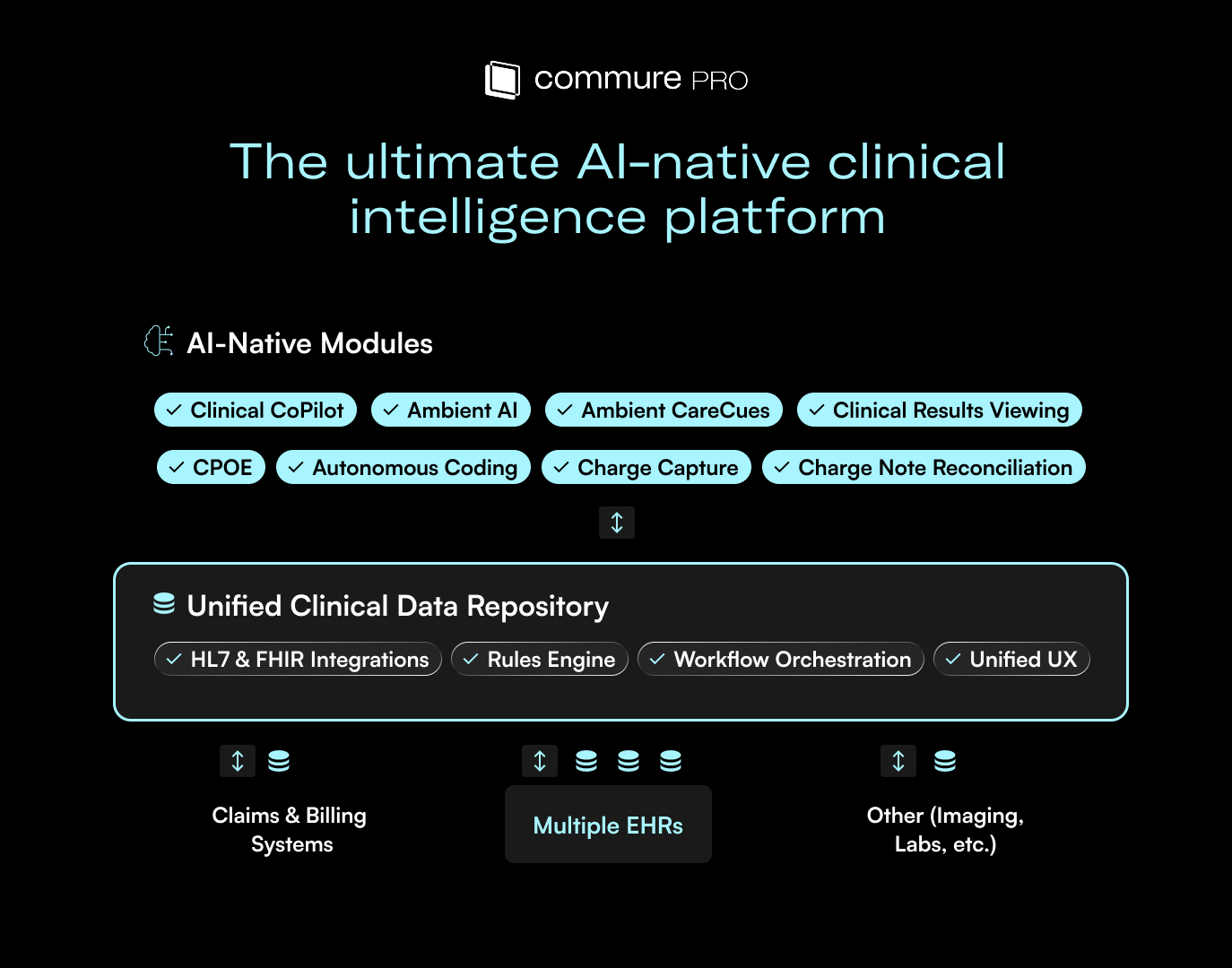
Co-Pilot and Autopilot: A Combined Model for Scalable AI
“One of the key emerging trends with AI in healthcare is that the tool functions both as a copilot and an autopilot,” according to Tandon. “One of the key emerging trends with AI in healthcare is that the tool functions both as a copilot and an autopilot,” according to Tandon. “Having both capabilities—copilot and autopilot—is, in my view, the dominant and defining trend we’ll see in healthcare over the next 24 months. It ensures humans are involved where they’re needed, and AI runs autonomously where it can."
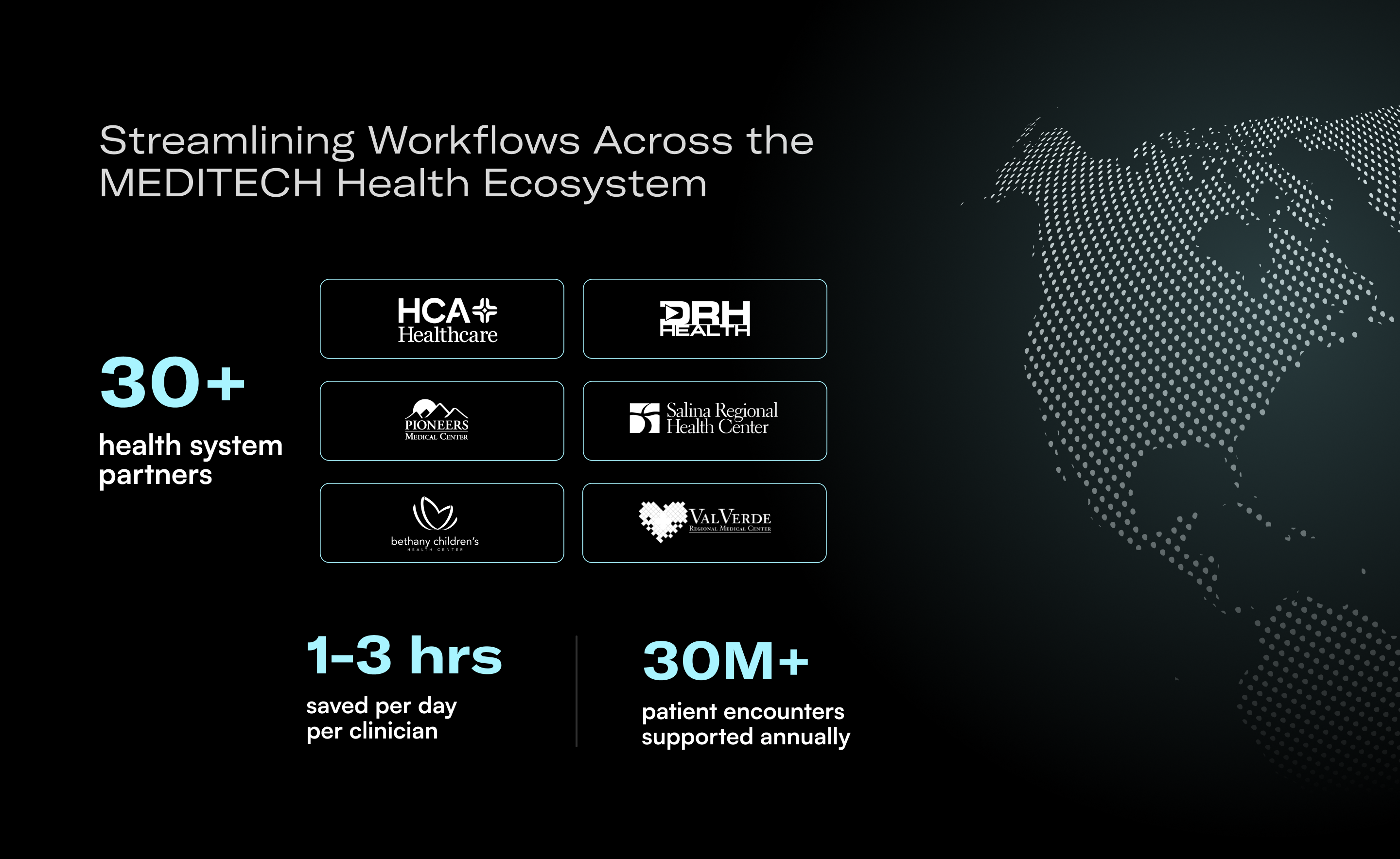
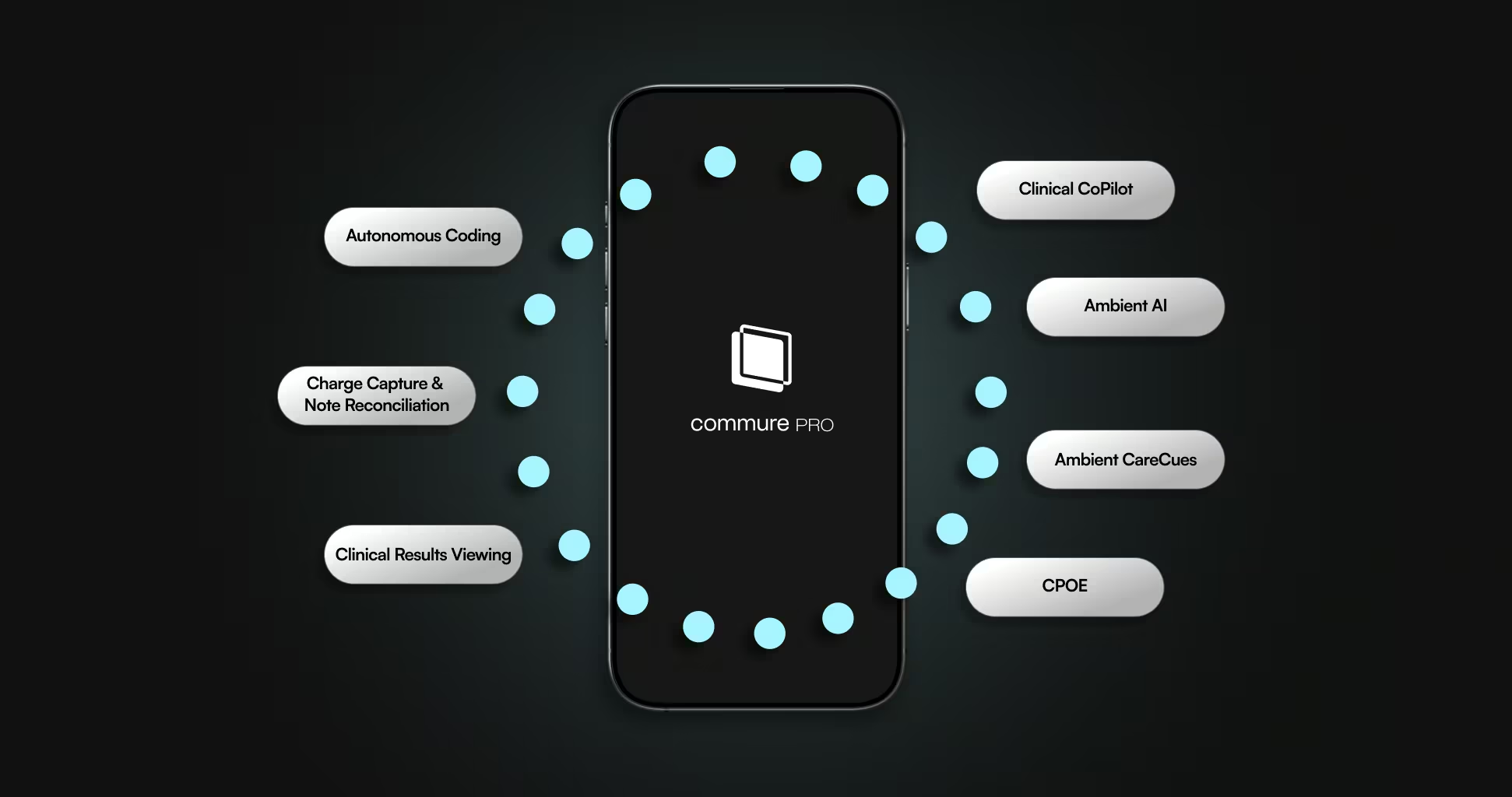
Commure employs a two-pronged approach to AI implementation. Some solutions function as assistants, requiring human validation, while others perform routine tasks independently, without direct intervention.
For example, Commure Ambient AI supports providers with clinical documentation during and after clinical encounters, across more than 25 healthcare specialties. Tandon shares, “For tasks where you want a human in the loop—where bedside manner, clinical context, and interpersonal dynamics matter—you want the physician present, with AI acting as an always-on assistant, listening and pulling information in real time, as a co-pilot.”
In contrast, Commure Agents enable fully automated workflows across administrative departments, such as front call centers, patient scheduling, and even denial management. “The beauty of the autopilot model is that it can run lights out, 24/7, freeing up time, resources, and capital without human intervention,” shared Tandon.
Ethics and Equity as Operational Requirements
“One of the most important problems in deploying AI in healthcare is ensuring that it's done in a way that is ethical and representative of all communities, that it's going to be used to treat,” shared Tandon.
Commure’s implementation methodology begins long before software goes live. Each system undergoes extensive simulated testing against historical clinical and administrative data to surface potential disparities or edge cases.
“One of the things we do at Commure is maintain a very stringent evaluation and testing framework. We virtually run, or shadow run, millions of previous appointments and claims before the technology ever touches a live patient in a health system," shared Tandon. "When done correctly, this means patients experience the positive benefits of AI from day one, instead of the chaos that often comes with other software rollouts.”
Putting the Brightest Engineering Minds on the Most Difficult Problems
Commure’s product development model intentionally brings clinicians and software engineers into continuous collaboration in order to ensure solutions are truly fit to any healthcare environment. Rather than requiring physicians to adapt to pre-built interfaces, Commure builds tools alongside clinical end users.
As Tandon explains, “Most software today within health systems was not built by providers, for providers. It was built by an IT team somewhere, and then providers were expected to comply with it. It was seen as a compliance and administrative burden and tool, as opposed to something that empowered physicians and nurses.”
Reflecting on Commure’s founding, Tandon added: “What happens when you bring together the best software engineers in the world with the best physicians, nurses, and clinicians—and have them work together to create magic?”
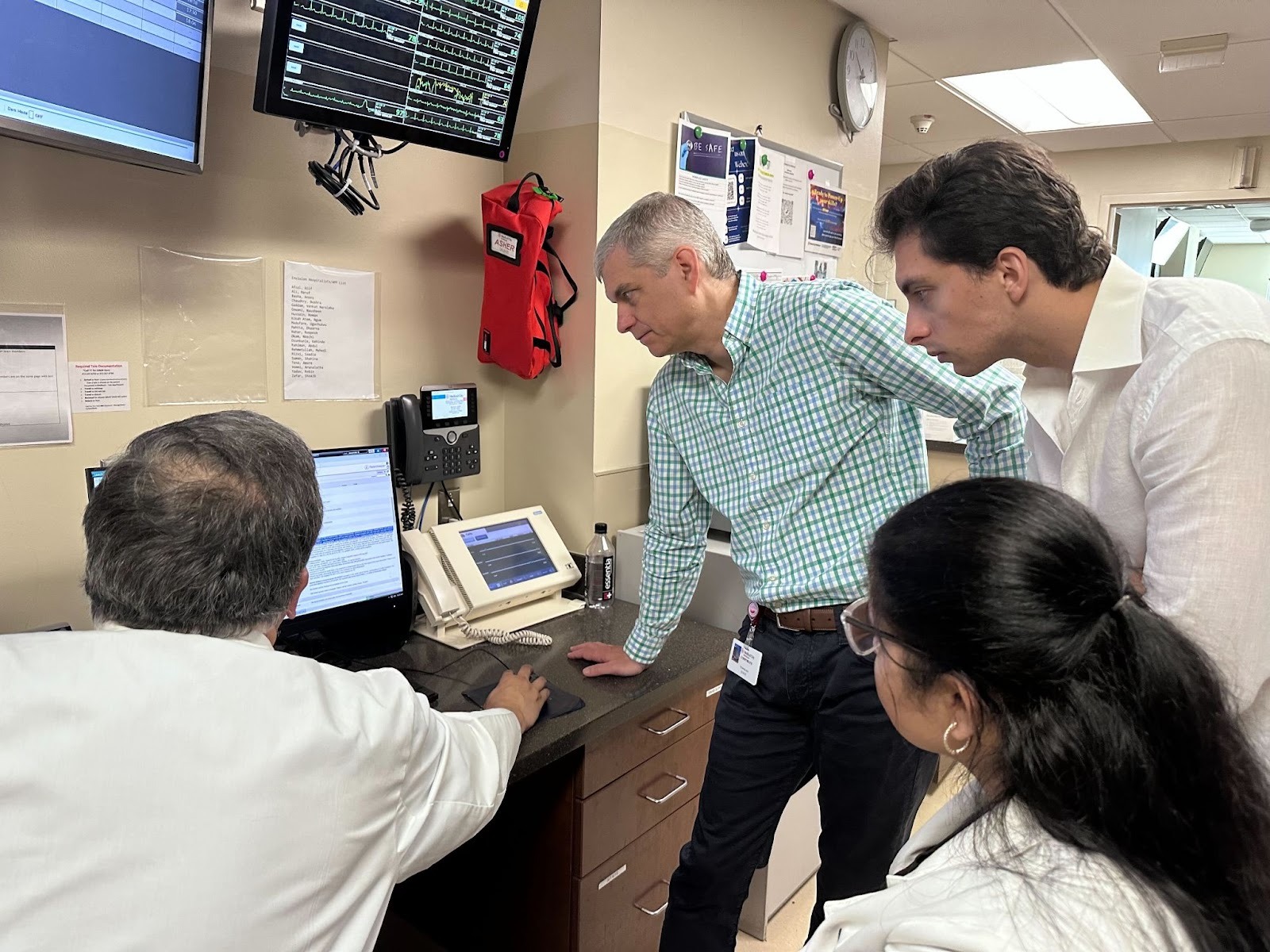
Commure’s Forward Deployed Engineering model embeds experienced engineering teams on site, enabling more context-specific, user-driven deployment and adoption.
Addressing “Work Tax” to Free Clinicians to Focus on Care
Ultimately, Tandon sees administrative complexity as the core barrier to clinician satisfaction and system-wide efficiency, sharing: “There’s often a lot of bloat work, or what we call a 'work tax' at Commure, that creeps into the day-to-day life of physicians and caregivers. That problem is at the heart of the healthcare system."
The long-term vision is not to replace the human aspects of care, but to elevate them by removing the background burden. As Tandon explains, “Where AI is heading in the next 5-10 years is a full-on transformation of how we do work and the types of tasks we focus on versus the tasks LLMs can take on on their own. An example of this, humans are best in class at: Empathy, caregiving, and the physical attributes of care, which is being there for a patient, understanding their conditions, making a diagnosis, and sticking through with it. Where AI is great is all of the work happening in the background.”
AI in both co-pilot and autopilot modes offers a powerful opportunity to reduce the unsustainable administrative waste in U.S. healthcare, freeing resources to drive innovation that makes care simpler, more seamless, and more affordable.
“Healthcare is a $4 trillion industry. At least $1 trillion of that is administrative waste. If we eliminated that and redirected a trillion dollars back into the U.S. economy, that’s non-inflationary stimulus every single year.”

.jpg)





.avif)

.png)