“Some providers may be hesitant at first, but once they start using it, they see how naturally it fits into their workflow. Ambient technology can adapt to any environment, and the key is to work with it rather than against it. When you do, it becomes a real partner in care delivery.”
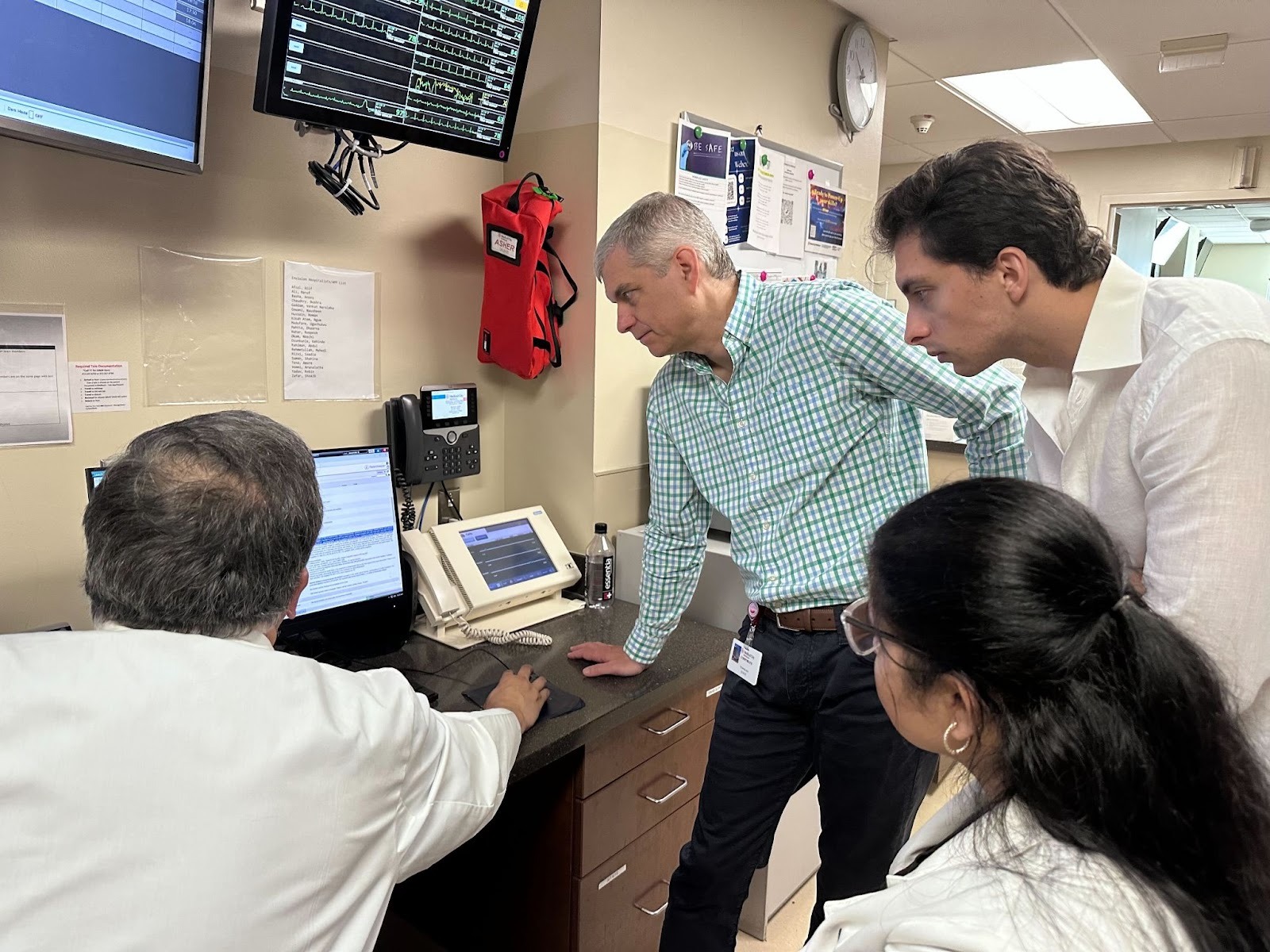
In this installment of Commure Uncharted, Dr. Jean-Luc Neptune, Executive Medical Director and member of the Commure Clinical Council, sits down with Sarah Wildermuth, Senior Operations Manager on Commure’s Enterprise Ambient Implementation Team. They discuss what successful AI deployments look like in the field, the lessons learned from large-scale rollouts, and the impact of Ambient AI on the provider experience.
A “Boots on the Ground” View from the Frontlines of Healthcare
Dr. Jean-Luc Neptune:
Great to speak with you again, Sarah. You’re one of our in-house experts on making Ambient AI work in the field. To start, can you tell us a bit about yourself and your recent projects at Commure?
Sarah Wildermuth:
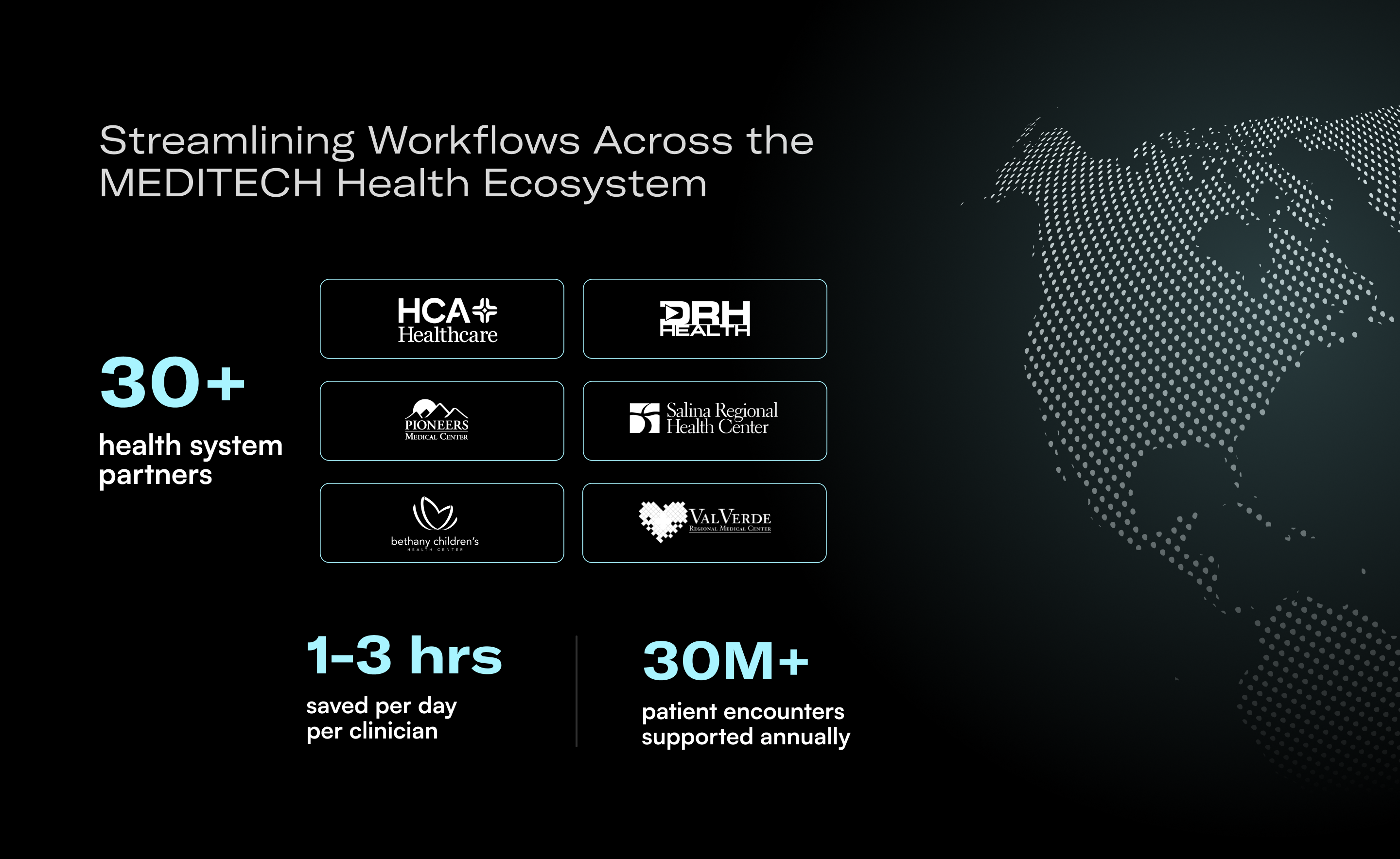
As a Senior Operations Manager on the Enterprise Ambient Implementation Team, I focus on enterprise-scale deployments across large multi-specialty organizations. Some of our most recent deployments have been with a 600-provider group and a 500-provider plus urgent care network. We are also beginning pre-planning with one of the largest health care facilities across several markets.
Each organization brings unique challenges. I have enjoyed learning those nuances and adapting our implementations accordingly.
We also manage pilot programs with providers ranging from tech-savvy early adopters to those who prefer a slower approach, which helps ensure the product works seamlessly for everyone.
What The Deployment Process Entails
Dr. Jean-Luc Neptune:
When working with a large national hospital chain that is rolling out new technology, what is step one? How do you even begin an engagement of that scale?
Sarah Wildermuth:
It starts with planning. We usually give ourselves a few months to prepare because you cannot just jump right in. Every department needs to know the project is getting underway, even those not directly involved in training, like revenue cycle teams. While they are not leading provider training, they see the downstream impact of better documentation and billing, so early communication is key.
We reach out to department leaders to let them know the project is happening and invite them to an initial kickoff meeting. That meeting covers timelines and an overview of the Commure Ambient solution, which sets the foundation for a smooth deployment.
Dr. Jean-Luc Neptune:
How do you align executives and frontline staff on expectations for new technology?
Sarah Wildermuth:
The most successful deployments start with strong leadership buy-in. Many of the executives we work with are clinicians themselves, so they have either tested the product personally or know colleagues who have. When they see the benefits firsthand, it makes a big difference.
When leaders champion the solution internally, it sets the tone. Providers are much more likely to engage when they hear directly from their Chief Medical Officer or another respected leader that the technology works and will help them. It creates awareness ahead of training and helps the deployment be received more positively across the board.
Dr. Jean-Luc Neptune:
For many providers, this can feel like new initiative number one hundred. How do leaders promote the real value of adopting Ambient AI?
Sarah Wildermuth:
We rely heavily on pilot programs. Before a full-scale rollout, we run time-bound pilots with a small group of providers who become our champions. They use Commure Ambient for several months, which allows us to gather both qualitative and quantitative data.
We measure things like documentation time saved, reductions in after-hours “pajama time,” and even improvements in E&M coding levels, especially in urgent care. When we share those results with the broader organization, it helps new providers see the tangible value from day one.
Dr. Jean-Luc Neptune:
Once the organization is aligned, what technical and operational steps must happen before deployment?
Sarah Wildermuth:
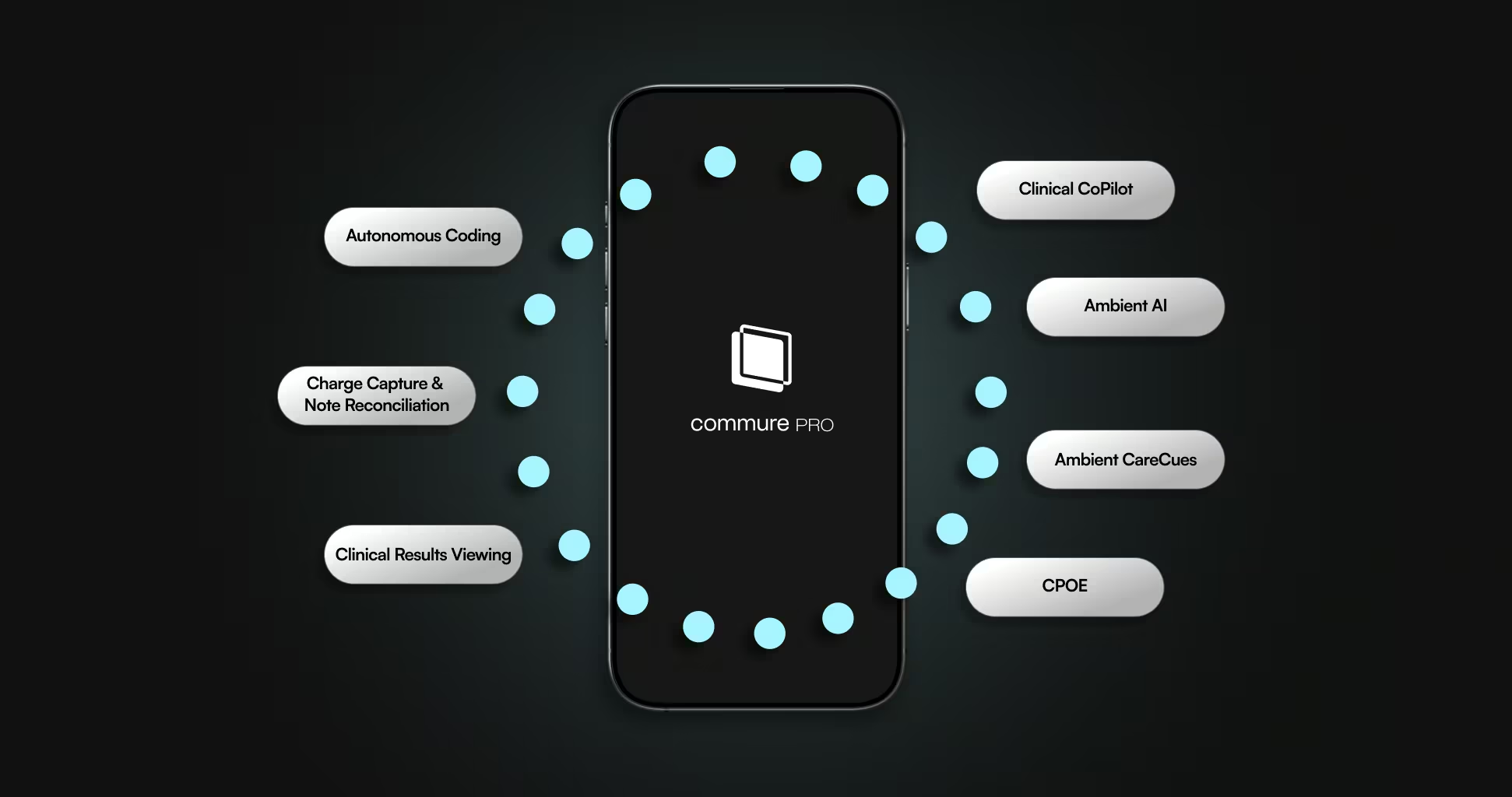
There is quite a bit happening behind the scenes. We start by integrating with the customer’s electronic health record, or EHR. That allows us to both pull and send information, which helps create a complete note with fewer clicks for the provider. Once the integration is live, they can generate and send their final note with a single click.
Alongside that technical workstream, we also have a compliance and security workstream focused on policies like data retention and patient consent. Then there is the provider operations and training workstream, which covers how we will train hundreds of providers over the rollout period.
In the best case, planning can be completed in about thirty days, depending on how quickly the customer moves. In more complex cases, it can take up to four months.
Evaluating Effectiveness & Impact
Dr. Jean-Luc Neptune:
When evaluating an ambient AI deployment, what metrics do you look at to determine whether it is working? And on the flip side, what are the early signs that something might be off track?
Sarah Wildermuth:
The main metrics are provider adoption and utilization. Adoption measures how many providers use Ambient AI at least once in a given day, while utilization tracks how often they use it across all their appointments.
If training completion is high but adoption is low, that is a red flag. It usually means providers do not feel fully confident using the technology. To close that gap, we conduct quick post-training surveys (just two questions via QR code) to assess readiness and identify anyone who might need extra support. We also run live test sessions in the EHR so providers can see the technology in action before they start using it with patients.
Dr. Jean-Luc Neptune:
And you also look at provider satisfaction and time savings, right?
Sarah Wildermuth:
Exactly. We track time-in-note metrics and conduct surveys to capture how the technology affects work-life balance and overall satisfaction. If providers are spending less time documenting, they are usually happier.
Burnout is a real issue in healthcare, and one reason I enjoy this work is seeing the direct impact on providers’ lives. We often hear stories like, “I got to pick up my kids from school today,” or, “I actually had dinner with my family.” Those moments are a reminder that the product really is making a difference. We are also implementing use cases for AI beyond clinical scribing, such as scheduling/front office workflows, appointment reminders and follow-ups, RCM, and much more.
Driving Adoption & Trust
Dr. Jean-Luc Neptune:
Some providers clearly love the technology and see the benefits right away. But there is always a small group who resist change. How do you build trust with that group?
Sarah Wildermuth:
Those providers usually take longer to become consistent users, but getting the technology in their hands is the first step. The platform is simple to use, and we handle backend setup so that the final note looks and feels like what they are already used to seeing. The goal is to reduce friction and make the experience as familiar as possible.
At its core, the workflow is straightforward: start recording, see your patient, end recording, and your note is ready. Once they realize how easy it is, they start to see the benefits for themselves. Even the most hesitant users often begin slowly, one patient at a time, but over a few weeks they build confidence and fully adopt it.
Dr. Jean-Luc Neptune:
What advice would you give healthcare leaders who are just beginning to prepare for ambient technology?
Sarah Wildermuth:
I would tell them that this technology is not going anywhere. One of our pilot providers put it perfectly when he said, “AI is not going to replace doctors, but doctors using AI are going to replace doctors not using AI.”
I have never seen a specialty or provider type where it does not work. Some providers may be hesitant at first, but once they start using it, they see how naturally it fits into their workflow. Ambient technology can adapt to any environment, and the key is to work with it rather than against it. When you do, it becomes a real partner in care delivery.






.avif)

.png)