Healthcare call centers are facing mounting operational pressure. Surging call volumes, rising patient service expectations, staffing gaps, cost constraints, and outdated infrastructure are all limiting their ability to respond effectively.
The operational impact is measurable. Average hold times now exceed four minutes, well above the 50-second industry benchmark set by the HFMA. Roughly 30% of patients abandon the call if they wait longer than a minute. And when they do reach an agent, only half of the issues are resolved on the first attempt.
Staffing is also a persistent bottleneck to meeting patient needs. Many centers operate at just 60% of their necessary capacity, and are particularly under-resourced during evenings and weekends. Labor accounts for nearly half of total call center costs, and because call volume scales linearly with staffing needs, increasing headcount quickly becomes cost-prohibitive.
Agentic AI offers solutions to automate high-volume, rules-based tasks such as scheduling, insurance verification, and routine triage. This helps healthcare organizations handle more requests with fewer manual steps, respond more consistently to patients, and stay available at all hours without adding staff.
What Healthcare Call Centers Handle Today
Healthcare call centers are no longer just support functions, they’re a core part of how patients navigate and access care within a health system. On a typical day, human agents manage thousands of inbound requests covering a wide spectrum of operational and clinical needs, including:
- Appointment scheduling and rescheduling
- Prescription refill and prior authorization requests
- Insurance eligibility and benefits verification
- Billing inquiries and payment support
- Referral coordination and authorization follow-up
- Nurse triage routing based on symptom severity
- General service questions (e.g., location, hours, provider availability)
Typically, these patient requests outlined above are not one-question calls. A single patient interaction often spans multiple categories, for example, rescheduling an appointment, verifying insurance coverage, and requesting a medication refill. Handling these requests typically requires agents to navigate EHRs, payer portals, and internal communication systems. Each added layer increases average handle time and the likelihood of handoffs or callbacks.
Increasingly, patients expect real-time service and seamless digital experiences. What was once a back-office support function has evolved into a high-volume, front-line service channel that demands speed, consistency, and the ability to scale with demand. Luckily, many of the tasks driving that demand are repetitive and rules-based, making them ideal candidates for automation.
What Tasks AI Healthcare Call Centers Can Automate
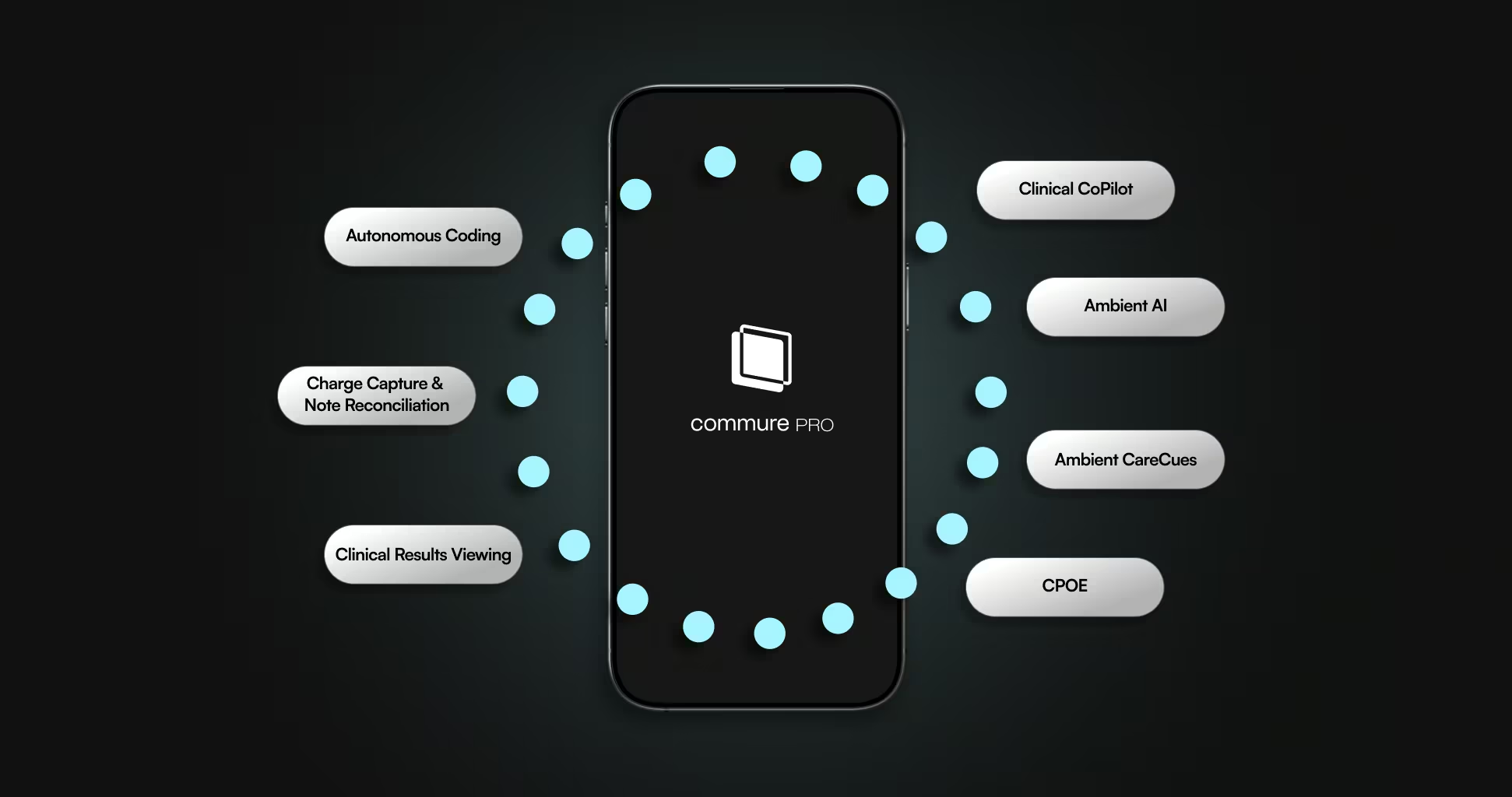
AI agents are not traditional chatbots or Interactive Voice Response (IVR) systems; they’re workflow-oriented tools designed to execute discrete, high-volume tasks across multiple systems without human input. Unlike traditional LLM-based AI technologies, AI agents can retain context across conversations, interact with third-party applications and data sources, and respond dynamically to real-time requests.
In healthcare call centers, their highest-impact use cases fall into a few key operational categories:
- Appointment Management: AI agents can schedule, confirm, reschedule, and cancel appointments by integrating with an EHR’s scheduling module. They support both inbound and outbound workflows, enabling patients to make changes via voice or chat. By automating these common tasks, health systems can reduce average handle time and lower the volume of follow-up calls resulting from missed or unconfirmed appointments.
- Prescription Refill and Prior Authorization Intake: Rather than routing refill and authorization requests to nursing staff, AI agents can collect relevant medication details from patients, initiate the request via structured forms or EHR-integrated prompts, and push the case into existing pharmacy workflows or prior auth queues. This streamlines medication access, freeing clinical teams to focus on more complex cases.
- Insurance Verification: Agents can interface with payer portals and eligibility databases in real time to confirm active coverage, identify copays, and check for plan-specific limitations. Depending on their configuration, AI agents can either retrieve information to assist a human agent or fully automate the eligibility lookup process, eliminating back-and-forth calls and manual portal navigation.
- Triage Routing and Intent Detection: Using natural language processing, AI agents can capture patient intent (e.g., “I have chest pain” vs. “I need a referral”) and match it to predefined routing logic. For flagged clinical terms or symptom combinations, they can escalate directly to a triage nurse or refer them to the emergency room based on the urgency. For non-urgent requests, they can direct the patient to self-service tools or begin the intake workflow.
- Follow-Up and Post-Visit Outreach: AI agents can initiate proactive contact after a visit, sending discharge instructions, satisfaction surveys, or medication reminders via SMS, phone call, or patient portal messages. They can track responses and escalate any red flags (e.g., patient reports worsening symptoms) to the appropriate care team.
These agents interact with EHRs, CRM platforms, payer systems, and internal scheduling tools in real time, either pulling in data to inform conversations or pushing updates based on patient responses. By taking on these repeatable, structured tasks, AI agents reduce the burden on human staff, accelerate response times, and allow organizations to scale without increasing headcount.
Beyond the Call Center: Expanding the Role of AI Healthcare Agents
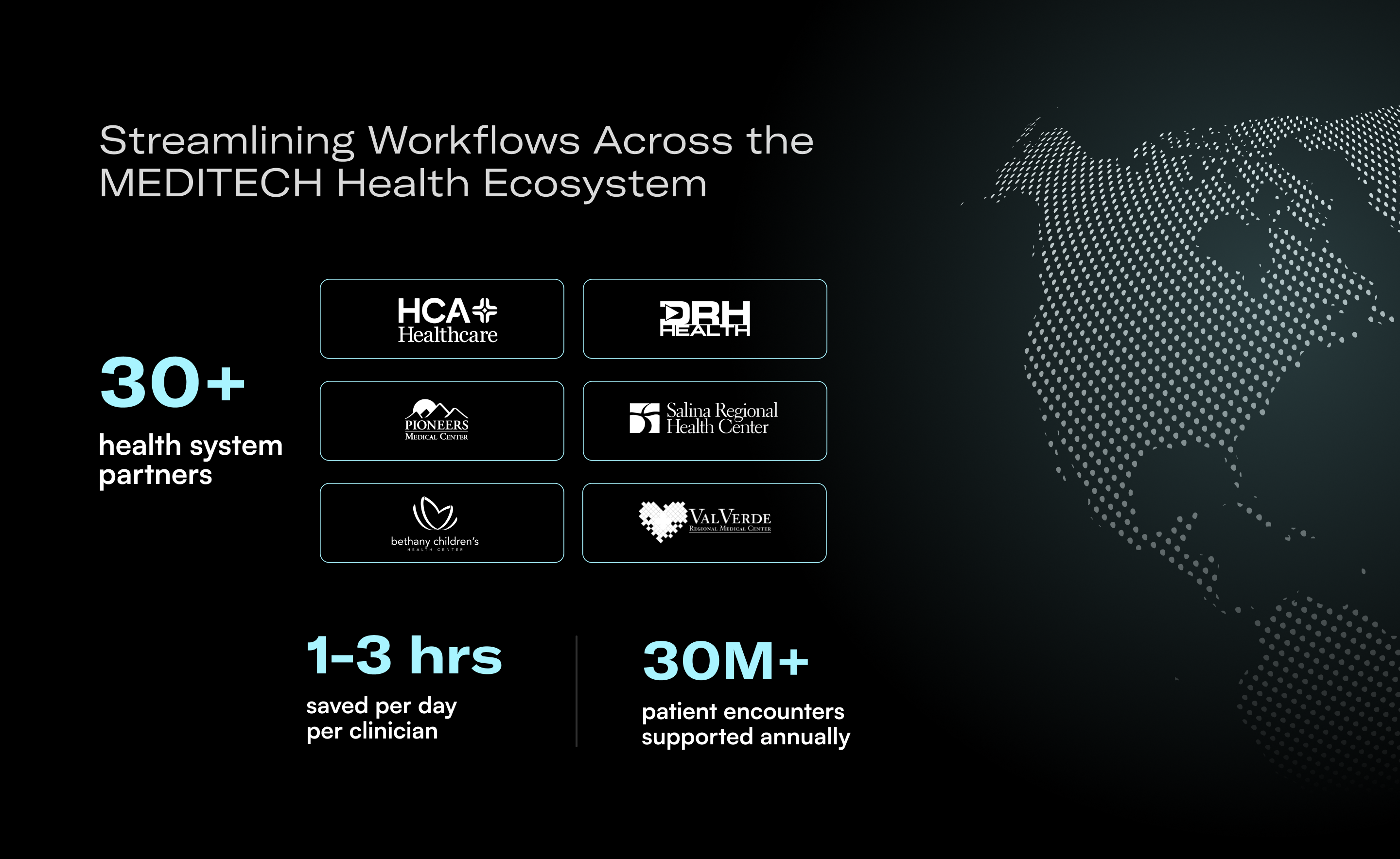
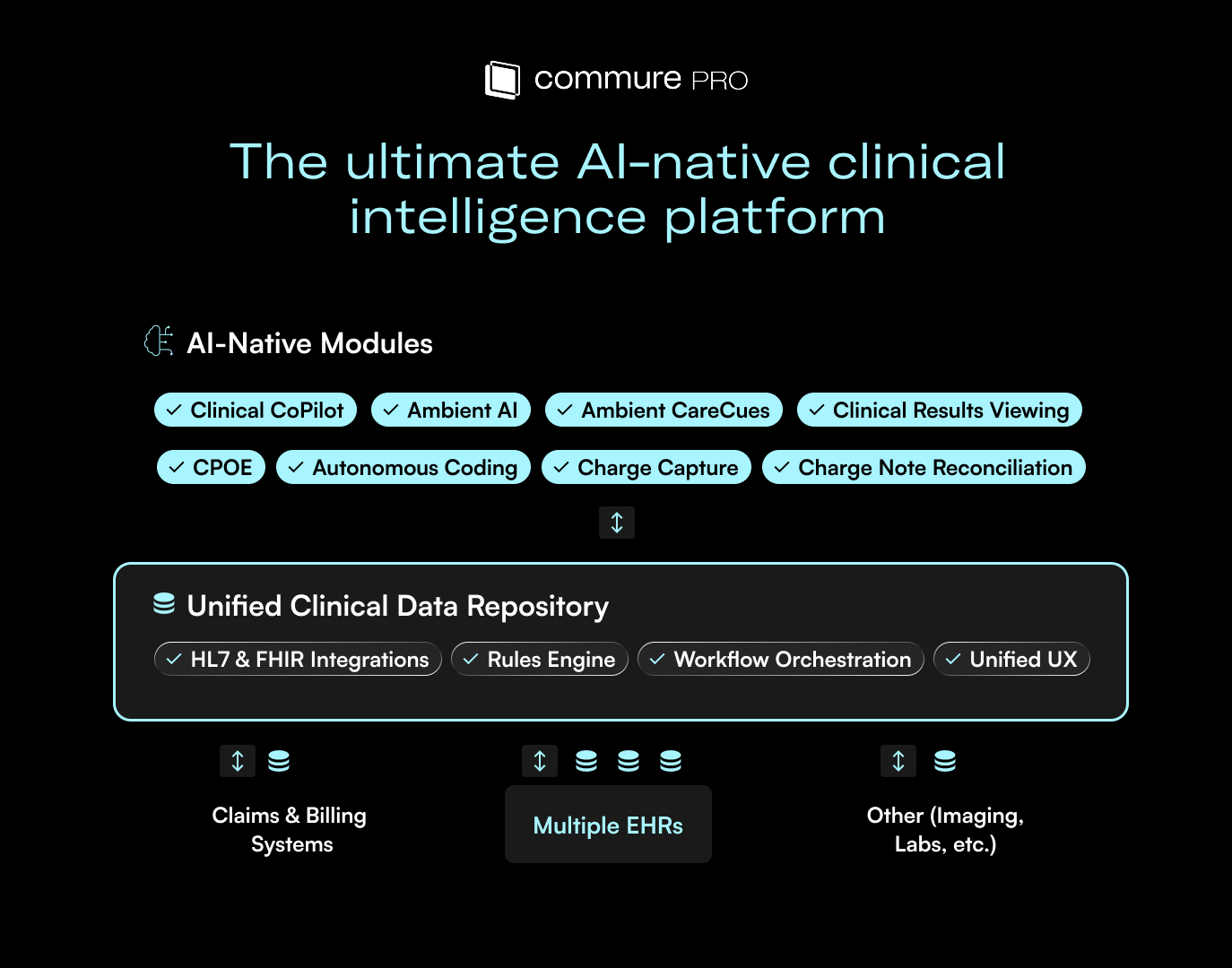
While healthcare call centers are a practical first area for health systems to apply this technology, the potential uses for AI agents extend much further. Commure offers a growing portfolio of agents designed to support operational workflows across patient engagement, revenue cycle management, and administrative coordination. Examples include:
- Denials Autopilot Agent: Supports denial management by identifying rejected claims, flagging likely causes, and preparing resubmission recommendations to accelerate appeal workflows.
- Claims Processing Agent: Automates repetitive aspects of the claims lifecycle, including status checks and reconciliation tasks, to reduce manual work and improve throughput.
- Payer Portal Agent: Retrieves documentation such as EOBs directly from payer portals, reducing the administrative burden on revenue cycle teams.
- Outbound Follow-Up Agent: Initiates post-visit check-ins to monitor recovery and adherence, with workflows that escalate issues to clinical teams when needed.
- Web-Based Benefits Lookup Agent: Gathers patient eligibility and benefits data from external systems, streamlining pre-visit verification and coverage checks.
Commure’s recent webinar with AWS showcased how AI agents can access real-time data, interact with external tools, and retain conversational context across interactions. These capabilities allow AI agents to coordinate tasks across disconnected systems, responding to real-time inputs rather than following static scripts.
Modernizing Healthcare Call Centers With AI
AI agents are reshaping how healthcare organizations deliver service across patient-facing and administrative workflows. Staffing shortages, rising service expectations, and increasingly complex payer and system interactions have exposed the limits of manual processes. Core functions such as scheduling, benefits verification, triage, and follow-up now demand levels of speed and consistency that are difficult to sustain with human agents alone.
By automating structured, repeatable tasks, agentic AI enables organizations to increase service availability, reduce operational overhead, and improve response time without expanding headcount. Agents maintain context across interactions, connect to external tools and data sources in real time, and coordinate workflows that span departments and systems. Rather than serving a single function, they provide a flexible operational layer that supports scale, accuracy, and resilience across health systems.
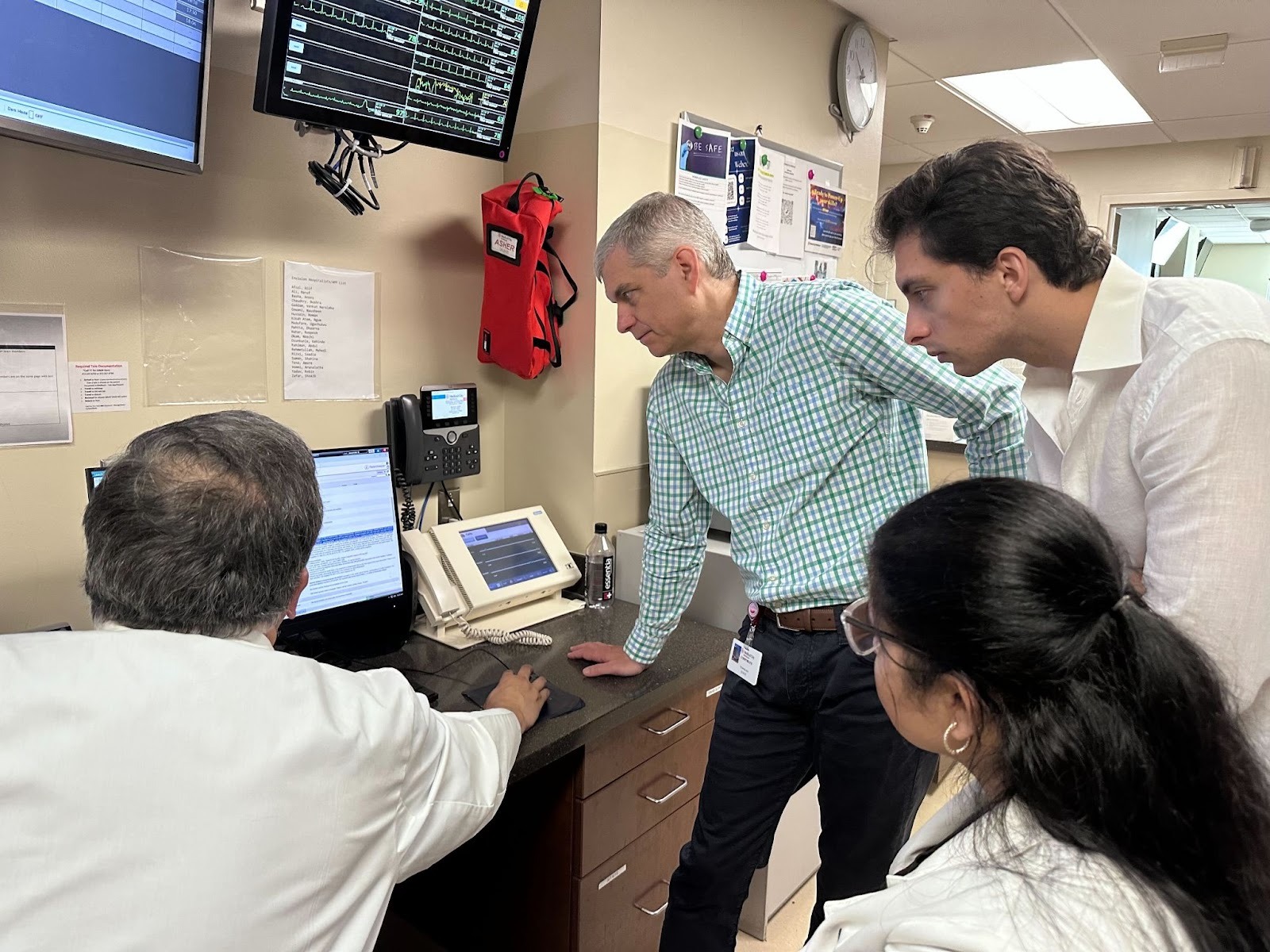
Commure supports this transformation with a forward-deployed engineering model, embedding technical experts directly within health systems to accelerate deployment and ensure alignment with existing workflows. This hands-on approach helps health systems move quickly from concept to production, minimizing integration friction and surfacing high-impact use cases early.
Ready to modernize patient operations with less overhead and more impact? Check out the Commure Agents product page to learn more or schedule a demo via the button below.






.avif)

.png)