“I was getting to the point where I was considering changing my career because I just had no life… I’m now incredibly happy. I left for a two-week vacation with absolutely nothing on the table and could walk away without any stress.” - Andrea Hazelton, FNP-C @ Pioneers Medical Center
This is just one of countless examples of clinicians across the country who are drowning in documentation, and how utilizing AI-generated doctor’s notes can help.
In fact, clinicians now spend an average of 16 minutes per encounter in the EHR, 11% of it after hours. Nurses report spending 19–35% of their entire shift documenting, a sharp increase from 9% in the paper era.
With this much time spent on administrative work, it's no surprise that 43% of clinicians report at least one symptom of burnout.
To add to that, health systems are under more pressure than ever to improve efficiency and maintain rigorous documentation standards. AI-powered doctor's notes offer a promising path forward. Here's what you need to know.
What Health Systems Should Expect From AI Doctor’s Notes
AI-enabled documentation is rapidly becoming a baseline capability. But as the market grows more crowded, the gap between commoditized features and enterprise-grade performance is widening.
For health systems, the real question is not whether to adopt AI-generated notes, it’s how to choose a solution that delivers measurable, system-wide value. That starts with identifying the operational outcomes that matter most:
- Reducing denial rates and billing friction
- Accelerating reimbursement through more streamlined claims
- Lowering clinician after-hours charting time
- Improving consistency in documentation across teams
- Scaling seamlessly across departments without heavy lift
Vendors may check the same boxes on a feature sheet, but implementation success and sustained value hinges on how well those tools work in reality.
Why Going Beyond Dictation is a Necessity
Legacy AI doctor notes tools still require clinicians to record their thoughts after the visit and often involve manual entry or editing. That workflow hasn’t kept up with modern clinical demands.
More advanced AI-powered documentation tools change the dynamic:
- Documentation starts and ends in the exam room: No need to circle back post-visit or piece together notes from memory.
- Every note reflects the full clinical picture: Tools pull in prior labs, diagnoses, and medications automatically.
- Nuance is preserved, noise is removed: Small talk is filtered out while clinically relevant cues are retained.
- Less screen time, more patient time: Providers can engage directly without toggling between note fields.
- Notes are directly integrated with EHRs and beyond: Structured output drives billing, coding, reporting, and workflow handoffs.
These advanced tools are already in use at leading health systems. At Dignity Health, providers using AI-generated documentation cut their charting time by up to 41%, freeing them to focus more on patient care.
What Health Systems Should Look For When Choosing an AI Doctor’s Note Solution
Not all AI-generated notes are created equal. Health systems evaluating tools should ask:
- Does the solution support multiple languages across diverse care settings?
- Does it support real-time documentation during multi-speaker conversations?
- Are the outputs structured enough to feed into coding, billing, and compliance systems?
- How fast can the platform be deployed and configured for different specialties?
- What clinician satisfaction or adoption metrics has the vendor demonstrated post-implementation?
- How customizable is the system for different note styles, specialties, and documentation templates?
- What level of human-in-the-loop quality control or review is included in the workflow?
- How transparent is the AI’s decision-making when it comes to clinical inferences or omissions?
Ultimately, to drive real impact, documentation tools must enhance, not complicate, how providers work day to day.
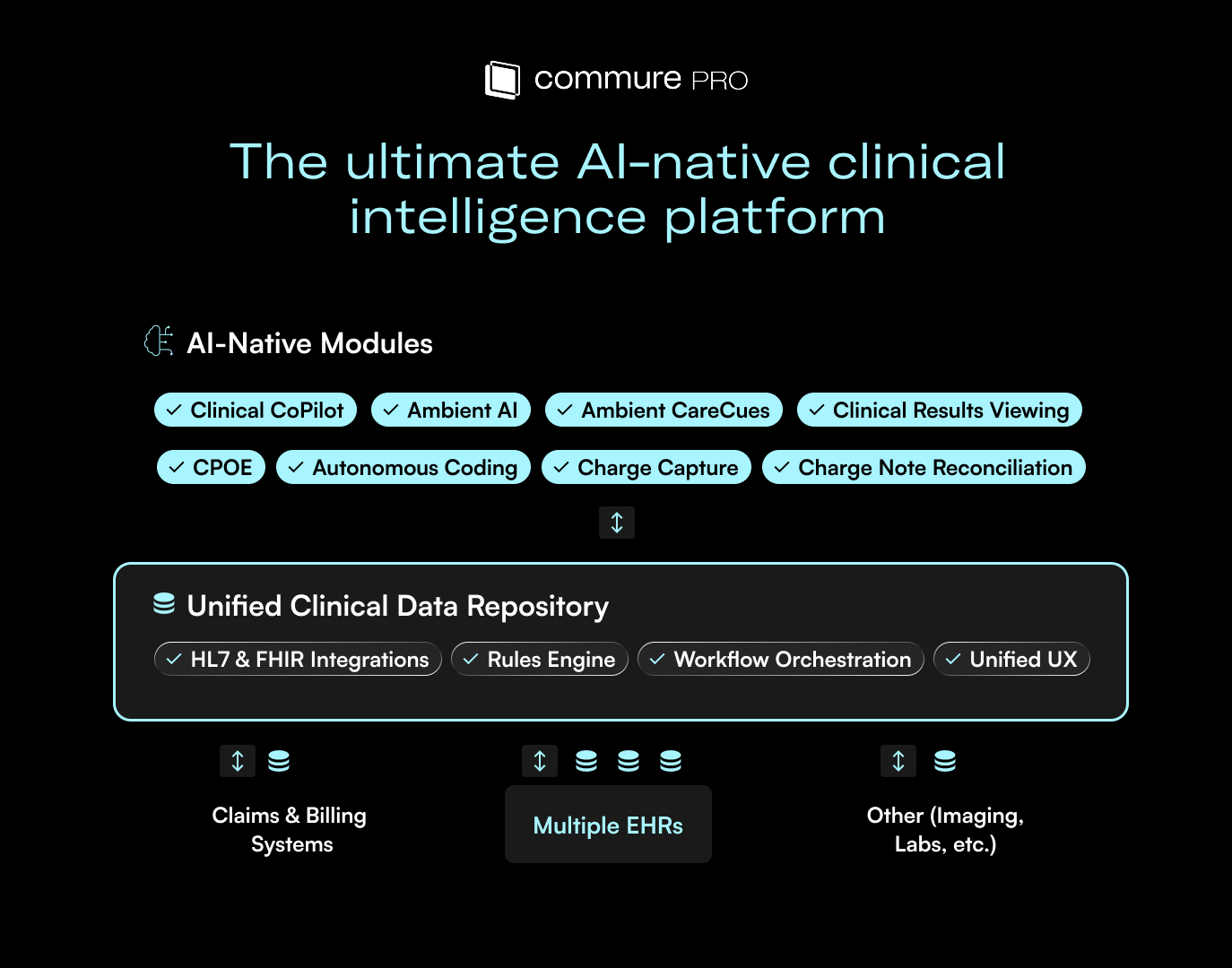
Commure Ambient AI is Built to Deliver at Scale
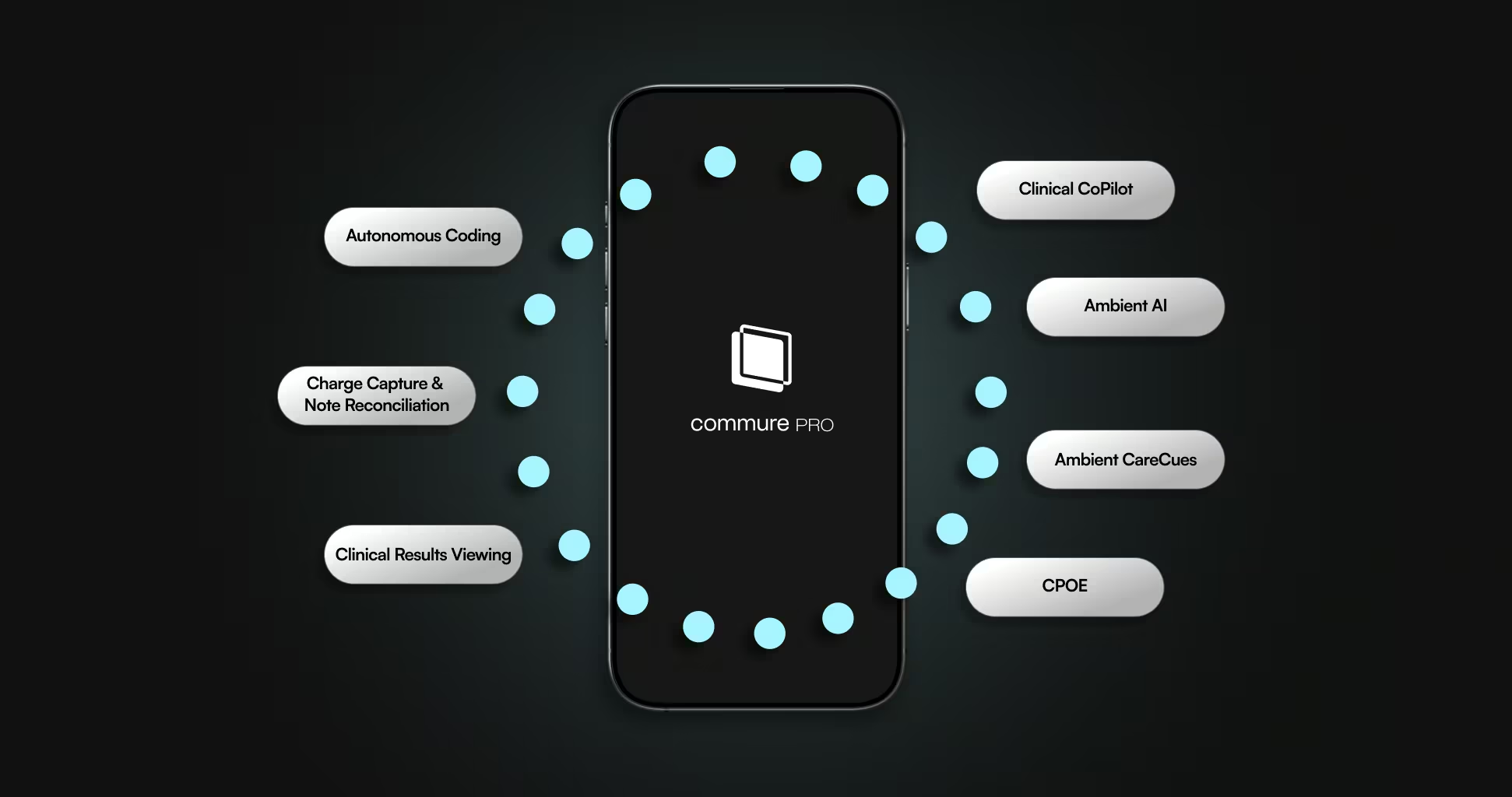
Commure Ambient AI moves beyond basic transcription by generating complete, structured, EHR-integrated notes without added steps.
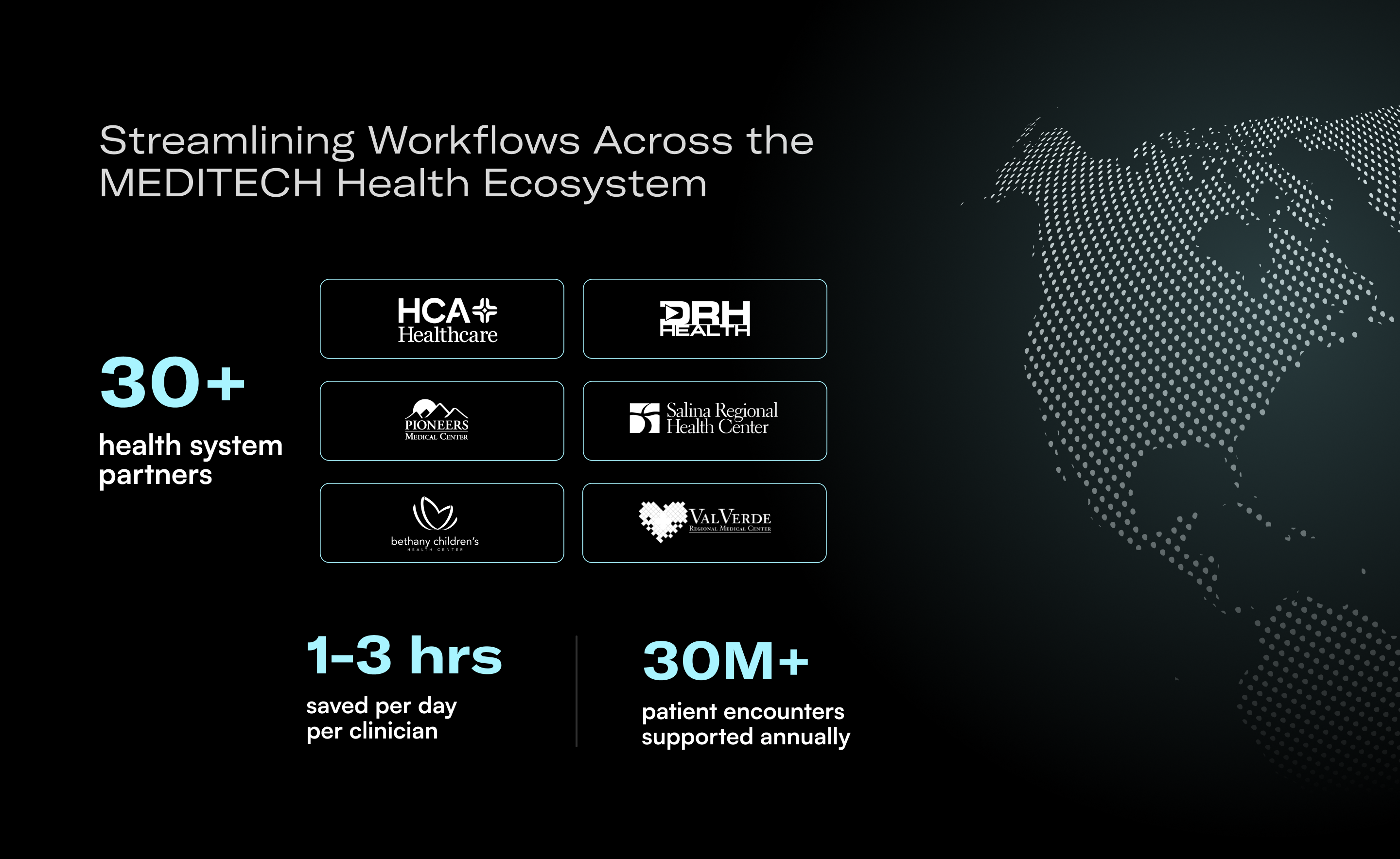
At Commure, health systems using Ambient AI report up to 81% less time spent on charting and a 25% drop in claim denials. That impact is driven by the system’s ability to understand clinical context, reference relevant history, and produce notes that are ready for coding, compliance, and reimbursement.
For health systems looking to modernize documentation, the goal should be better outcomes through streamlined workflows. Ambient AI offers a path to scale efficiency and quality without adding complexity.






.avif)

.png)