Care doesn’t end when the IV comes out and the telemetry monitor is silenced. Once patients leave the hospital, most of their recovery plays out at home, where daily choices and limited support determine whether care plans hold or drift. The journey spans far more than a series of visits, and the handoff between settings shapes everything that follows.
For years, the default response was to add people and stretch shifts to cover every detail of discharge. Unfortunately, that approach almost always breaks down under staffing shortages, constrained resources, and slipping engagement.
What is needed now is a smarter layer of support that helps teams guide patients through the days and weeks after they leave. With the right technology, instructions carry forward, risks surface sooner, and transitions become easier for patients and clinicians to navigate.
What are transitions of care, and what are the risks?
Transitions of care are the handoffs between settings in a patient’s journey, like discharge from the hospital, a move to rehab, or the shift to at-home care. These moments are vulnerable. One study found that nearly 20% of patients experience adverse events within three weeks of discharge.
Another large contributor to failed transitions is handoffs between providers. One study showed the likelihood of 30-day hospital readmission increases by 16 percent with just a single handoff, and one in four hospitalizations during home health care could be avoided if handoffs were eliminated.
When handoffs falter, care teams feel the strain. Workloads rise, scarce resources get stretched, and frustration grows as avoidable issues return to the front door. The result is less time for top-of-license work, weaker communication, and a higher chance that small problems escalate into patient harm.
How can transitions of care be improved?
To fix transitions, start with why they break down. Discharge information is often incomplete or hard to follow, which leads to missed medications, drift from the care plan, and preventable readmissions.
The strongest lever to combat this breakdown in care is standardized, clear communication at discharge and across settings. Studies have found that communication interventions at the point of discharge are strongly associated with fewer readmissions, as well as better treatment adherence and patient satisfaction.
However, conversation alone is not enough because patients forget more than 50 percent of what is discussed. It is important to reinforce instructions with timely reminders and anticipatory guidance delivered where patients will actually see and use them.
How can digital healthcare help with transitions of care?
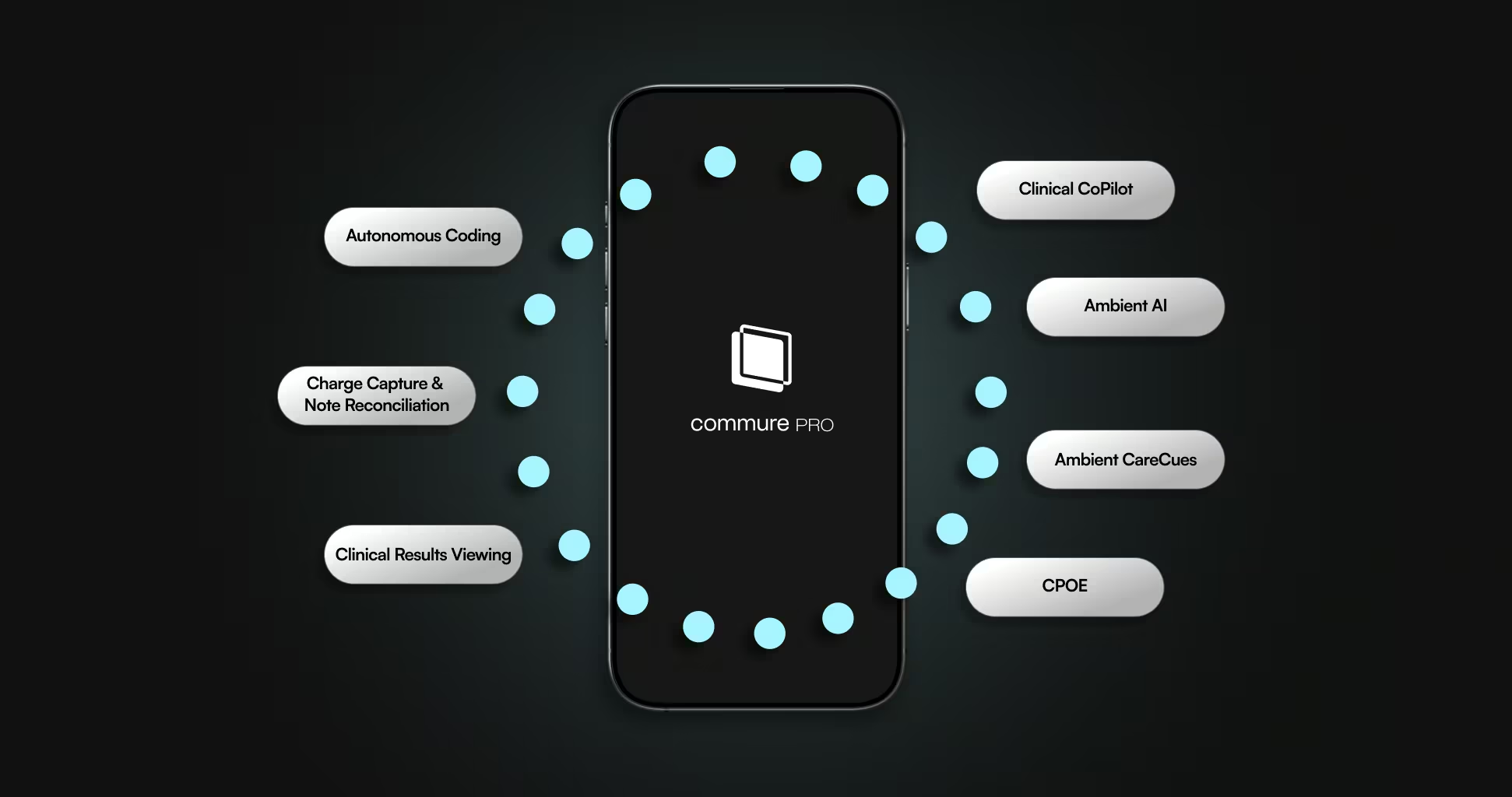
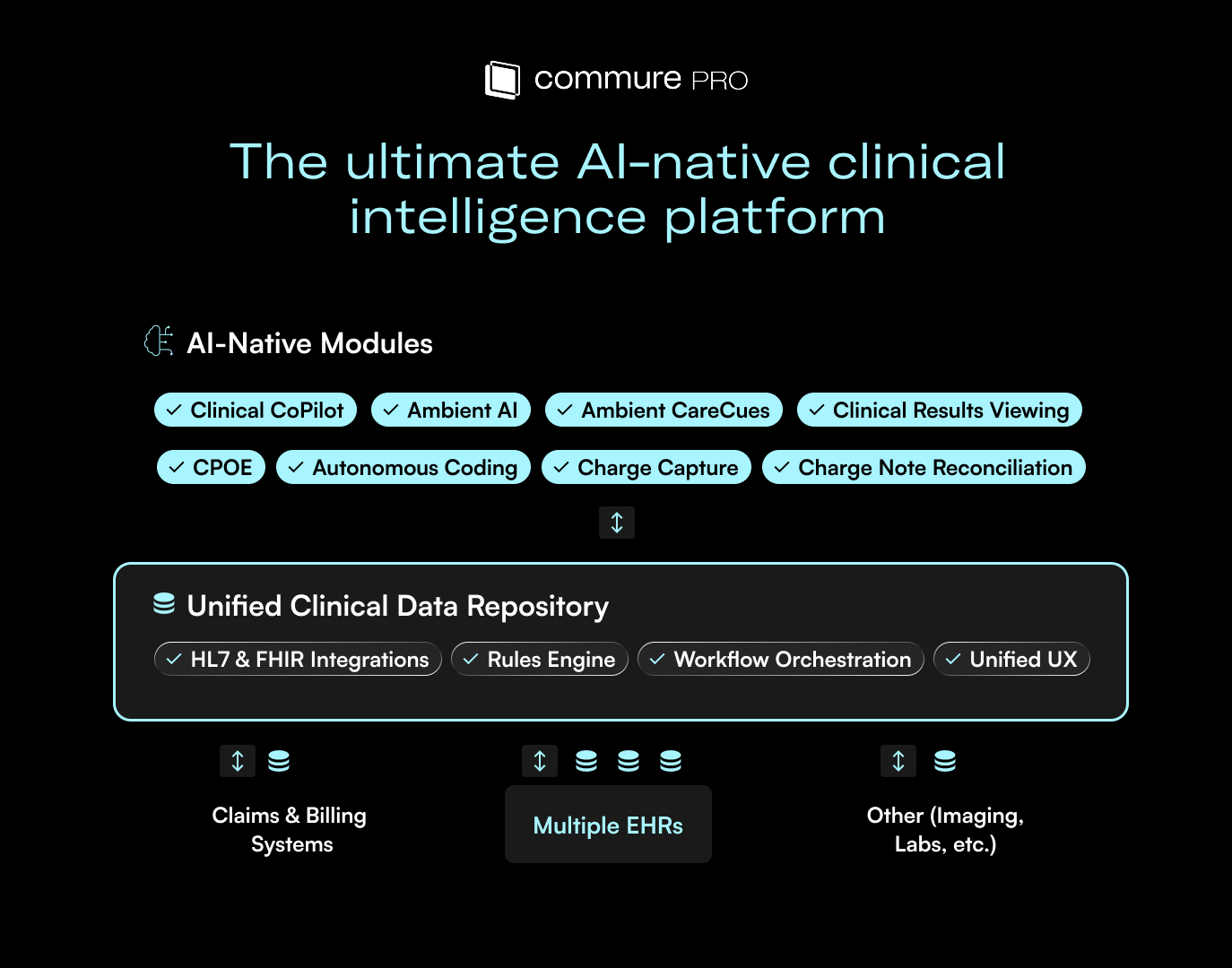
Closing the gap after discharge takes more than a conversation at the bedside. An intelligent care enablement platform gives patients and clinicians continuous support as care moves from hospital to home. Here is how they can help:
1. Streamlining care coordination
A unified view of the patient’s journey helps teams act quickly and consistently. With Commure Engage, clinicians can see patient messages alongside history and prior touchpoints, then loop in the right colleagues from an EHR-integrated workspace so nothing gets lost between settings.
2. Automating care follow-up
Refills, check-ins, and reminders are essential yet time-consuming when handled manually. Automation ensures every patient gets timely outreach and symptom checks, while clinicians spend more time at the top of their license and less time chasing tasks.
3. Educating patients
Discharge education fades fast. Conversational AI keeps teaching alive after the hospital stay by answering plain-language questions, reinforcing critical steps, and guiding patients to next actions with clinically reviewed content.
4. Simplifying symptom management
New or confusing symptoms often drive unnecessary calls and readmissions. A virtual assistant can respond in real time, ask clarifying questions, and escalate to the appropriate clinician when needed, giving patients clear direction and care teams actionable context.
5. Improving remote patient monitoring
Once patients are home, visibility drops. SMS-based outreach meets people where they are, captures status through brief check-ins, and flags issues early. That reduces back-and-forth in portals, clears up miscommunication, and keeps transitions moving in the right direction.
Ready for smoother transitions of care?
Every organization has its own hurdles, but the fix begins with clear communication and a platform that keeps guidance consistent from bedside to home. Commure Engage was built to do exactly that, so patients land on their feet and care teams stay aligned.






.avif)

.png)