“There was a lot of worry that patients would not accept being recorded [with Ambient AI]. However, after many conversations with leaders across the country, we generally see the opposite. Patients are usually on board and acceptance rates are 95% or higher.” - Donald Lazure, PA, Enterprise Clinical Strategy Lead
In this installment of Commure Uncharted, in-house clinical SME, Donald Lazure, PA, speaks from personal experience on bringing AI into the exam room without losing patient trust and what’s driving adoption amongst providers.
Q: Let’s start with data privacy and security. Providers are hearing concerns about AI from patients, including potential HIPAA violations, breaches, and unclear vendor data handling practices. How should providers address these concerns?
Donald Lazure:
As a provider, you lean on your organization and IT team to vet this. They need to dig into where the data is stored, onshore or offshore, what type of cloud is used, and the overall architecture.
The other piece is authorization and access, who should see the data and at what level. Any AI platform should let you tailor authorization to individuals and roles. A medical assistant may need a different view of PHI than a PA or an MD. Your office IT staff may not need PHI at all. This allows people to work at the top of their license while protecting privacy.
In Epic, for certain psychiatric notes, there is an extra security step to confirm you actually want to open that record, in case you mis-click. All this being said, these are valid concerns that people have, and they definitely need to be evaluated and vetted when bringing on an AI healthcare tool.
Q: Some patients may feel uneasy about being recorded during a visit. Should they be apprehensive, and how do you ease those concerns?
Donald Lazure:
I have been in the ambient AI space for a few years now. Early on, there was a lot of worry that patients would not accept being recorded. Across a couple of companies I’ve worked for and many conversations with leaders across the country, we generally see the opposite. Patients are usually on board and acceptance rates are 95% or higher, which has been a pleasant surprise.
Should there be some caution? Yes. Technology should be vetted and used appropriately. Large language models are being fine-tuned for healthcare with guardrails so they do not reach out to the entire web. Hallucination rates have come down, and models are better at contextualizing the conversation and the information collected. Patients also see AI more in daily life now that ChatGPT is widespread, so it feels like a normal technology advancement. I do not see this as a major stumbling block on the patient side, and I am happy about that.
Q: What does it look like when ambient AI fits well into provider workflows?
Donald Lazure:
The North Star is you walk into a room and speak, the system knows who is there, picks up voices, maybe even notices facial expressions or hand motions, and can act on what is said. We are not there yet, but we are a lot further along that path than I would have guessed five years ago.
A good integration lets the clinician care for the patient better by bringing the right information to the forefront. It adds clinical insight and context from past history without making you dig through the EHR, health information exchanges, lab portals, and everything else.
It also helps with decision-making. It can surface evidence-based guidelines and flag things like a medication that should be changed because of a QT prolongation on the last EKG or a drug interaction in the medication list. That kind of cue is better before the order is placed, so you do not have to undo work. And then everything needs to land in the EHR cleanly. The EHR is still the record of truth, so the ambient capture should flow in appropriately and simply, without extra steps and clicks.
Q: From your conversations with other providers, what tells you these AI tools are working—and what red flags make people pause?
Donald Lazure:
The strongest acceptance comes from clinicians who actually use ambient technology regularly. They report amazing satisfaction, reduced cognitive load, reduced burnout, and, depending on the level of integration, faster completion of encounters.
On the revenue cycle side, you generally see an uptick in what gets captured because clinicians are now documenting the full scope of work. Notes are more robust, so you are appropriately billing for what happened, whereas very short notes limited what you could code.
Where people hesitate when it comes to adopting ambient AI tools is integration. If it writes a great note, but I have to copy and paste sections into different parts of the EHR, then edit in multiple fields, it slows me down. If it does not bring additional care cues or past medical context to the forefront and only captures the moment in the room, there is still a lot of work to get it into the EHR. When integrations are not up to par, adoption drops because it feels like a slowdown.
Q: What needs to change in the EHR and vendor ecosystem to unlock real progress with AI?
Donald Lazure:
As EHRs roll out their own AI tools, I worry that limiting interoperability with software vendors will choke off R&D. Sometimes, there is a deal with a smaller company. Other times, the EHR builds it. They do not have the time and energy to match what startups in places like Silicon Valley and Boston are putting into health AI. I would hate to see innovation slowed because startups do not get the opportunity to plug in.
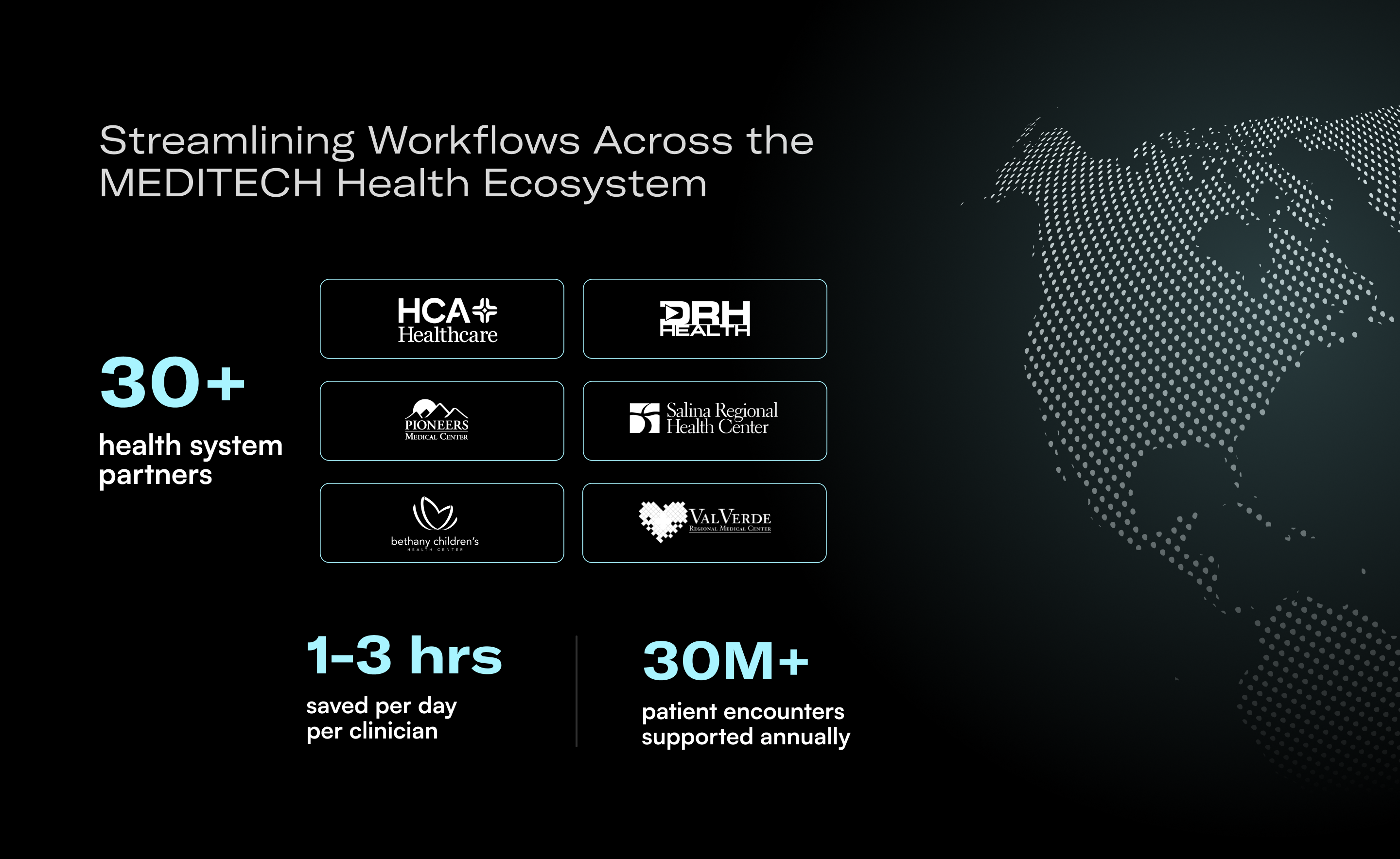
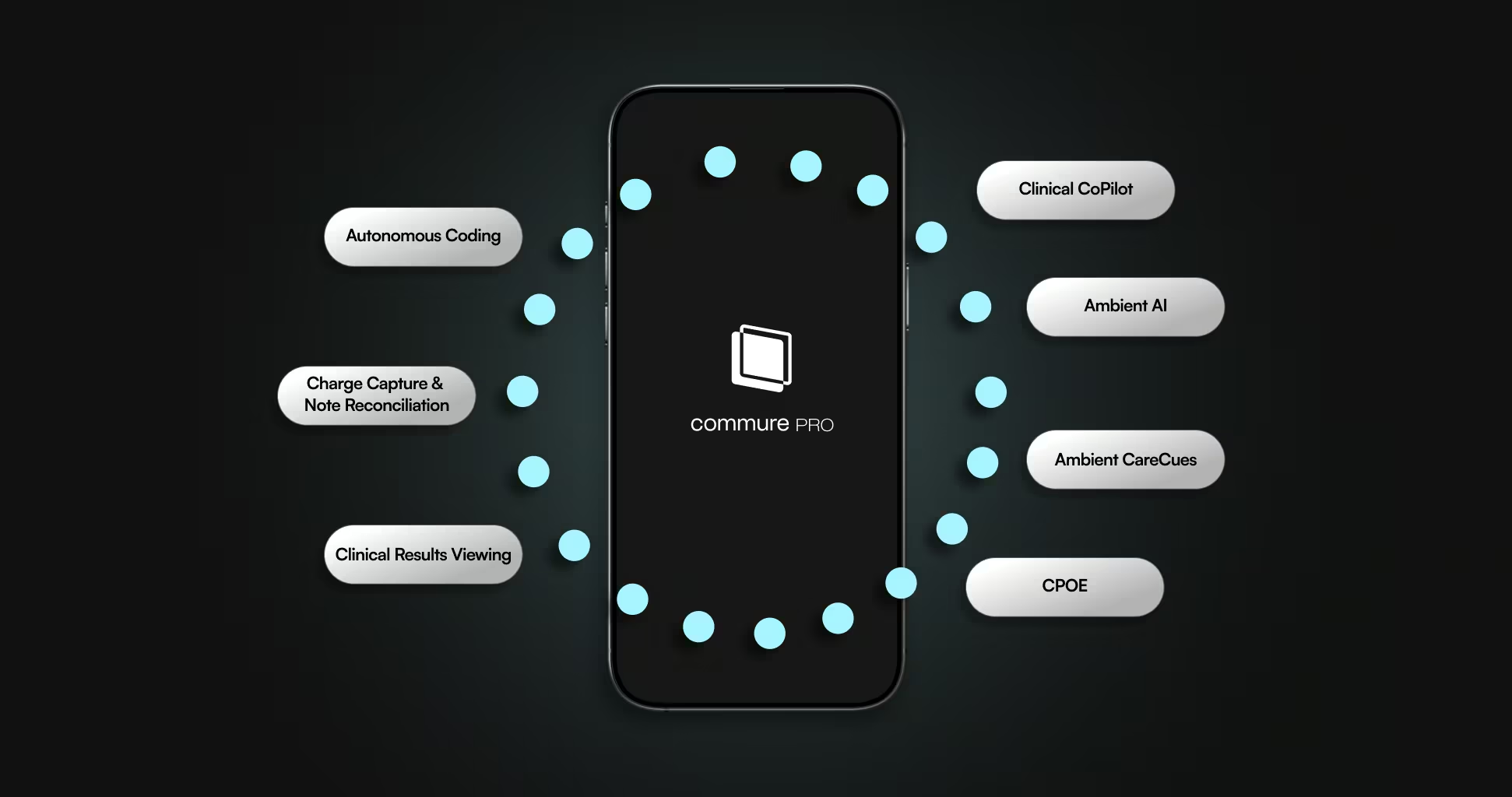
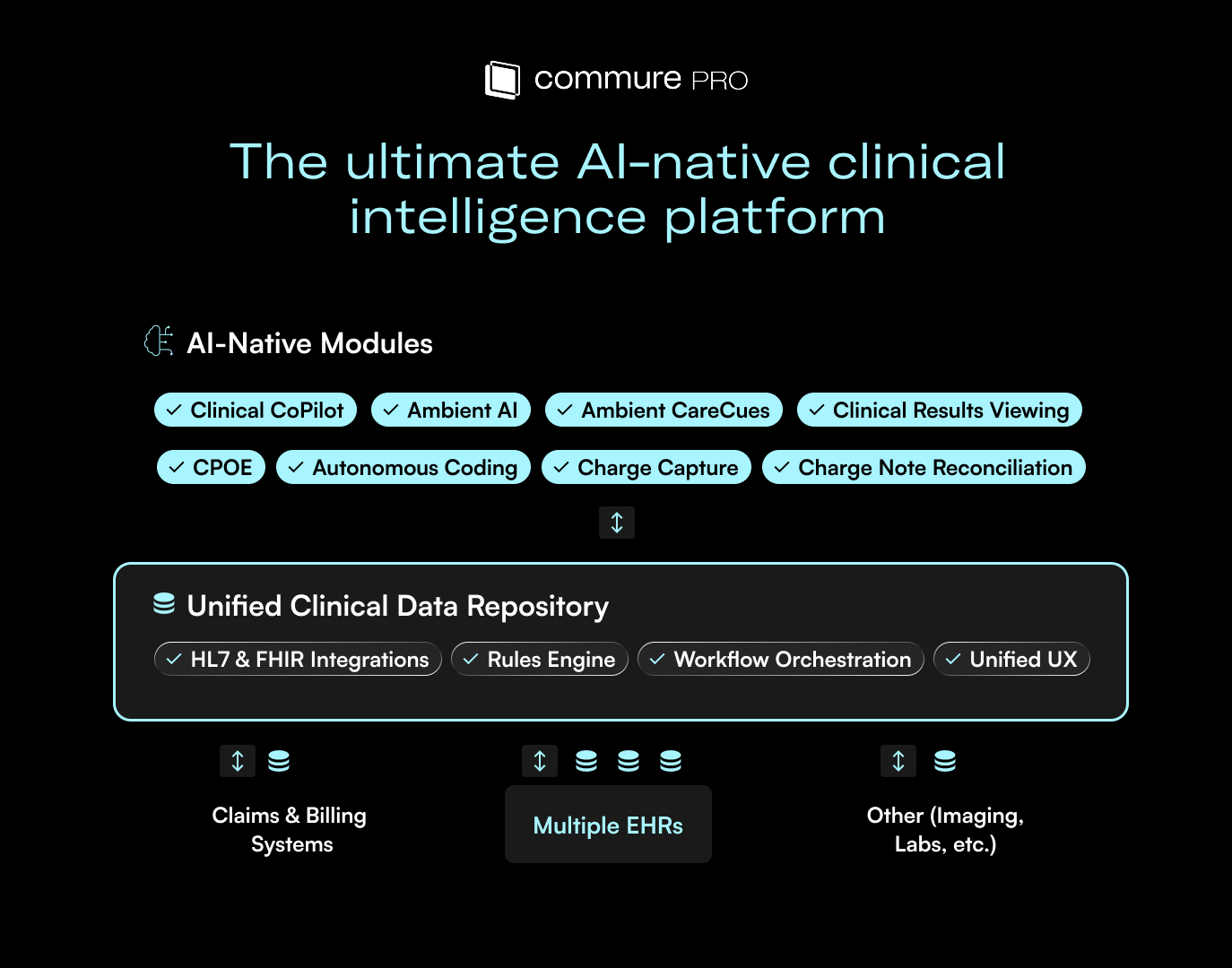
We also need to move away from point solutions. That is a big part of Commure’s premise: support the patient journey end-to-end, from first contact through discharge and financial clearance, with pieces that work together. Otherwise, you end up with small tools that do not talk to each other, and care gets piecemeal.
I would like to see stronger interoperability across startups, health systems, and existing tools. Give us a common code structure and a shared platform so these systems can speak to each other in context. Then everyone can do their best work in their lane and still connect across the choices a healthcare organization makes.
Q: “Change management” gets used everywhere. In healthcare, what does it mean, and how can it help health systems adopt AI with confidence?
Donald Lazure:
Change management can be individual, departmental, organizational, or even global. At the global level, it is asking why we keep doing things the way we do today. Why does the EHR have to be the record of truth? Could we capture everything in a database and query it with generative AI? Do we really need discrete fields, APIs, and HL7 feeds forever? Maybe each patient could have their own database. In a far-off future, that could even be something like a chip under your skin that you scan so the system can query it. That is way down the road, but it would be beautiful.
At the user level, I see this with some surgeons. They run from case to case and try to squeeze in clinic patients in between. They do not want to spend five or ten minutes learning something in the current EHR that might save them hours later. They just want to get it done the way they always have. A practical driver of change is seeing colleagues in the same specialty adopt a tool, get out of the office on time, and enjoy their work more. Getting a few key people to pilot and then show results to their peers goes a long way.
At the organizational level, change management is hard because you need IT resources and upfront spend on services and configuration. You make adjustments now and hope to see ROI later. That return is not always money. It can be better patient care and improved staff satisfaction. Those benefits matter, but they are harder to measure, which is part of why change management is difficult.
Q: As pressure mounts to justify AI investments, health systems are taking a harder look at where ambient AI can drive measurable value. Where should they focus?
Donald Lazure:
It is often a long-term gain. It is rarely one line item or one role you no longer hire. What you do see is happier end users, less cognitive burden, reduced burnout, and better retention. That is a hard ROI to pin down because you do not know when someone would have left. I have seen it quoted that hiring and ramping a new physician can cost around a million dollars to reach full productivity. That is a big number, but proving it out takes years.
You can measure revenue tied to more complete documentation. Compare providers using ambient to their own prior period, or to colleagues who are not using ambient, and look at captured revenue. That requires pulling data from the clinic, the revenue cycle team, and finance, which makes the analysis harder because it spans multiple stages of the patient journey.
There are time metrics like minutes spent creating a note, but those can be misleading. If a provider leaves the EHR open in a note field while multitasking, the time capture is not accurate. It is common to leave a note open, which is why those metrics can be tricky for ROI.
Q: Ten years from now, if we have a very advanced AI doctor, what role will humans play in care?
Donald Lazure:
It all depends on how patients receive this new technology. We could automate AI in certain instances, like low-level urgent care or for people who cannot make it to an appointment. But the clinician-patient relationship is meant to be ongoing. There is empathy, understanding, and education that we perform as humans. AI is getting better in that respect, and there are studies that say AI can score higher on empathy. So we will see. A lot comes down to patient acceptance. In a future state, one clinician might manage a few different agents that see patients, while the clinician provides oversight across multiple patients at once, which could be a realistic next step.






.avif)

.png)