Tell us a little bit about yourself.
My career began at Goldman Sachs in Salt Lake City, and shortly after New York City, where I drove global digital marketing and event strategies for the investment and private wealth management divisions.
From there, I moved into management consulting at Ernst & Young (EY) in San Francisco, where I helped build the digital transformation practice. I developed new service offerings, led multimillion-dollar client pursuits, and delivered executive workshops on emerging technologies. One of my proudest accomplishments and what initially sparked my passion for healthcare was launching an award-winning website and digital content strategy for the new Kaiser Permanente School of Medicine.
Eventually, my passion for healthcare innovation led me to a Head of Marketing role at Augmedix, a publicly traded SaaS company focused on ambient AI medical documentation. I oversaw the brand strategy, corporate communications, as well as built and executed a multi-channel marketing strategy that generated an annual $20M+ pipeline and fueled 40%+ YoY growth. It was an amazing journey to be with Augmedix from Series B all the way through IPO and eventual acquisition.
In October 2024, Augmedix was acquired by Commure, where I now lead PR and communications. I’m energized by the mission to transform healthcare and excited to help tell Commure’s story to the world.
As a kid, what did you want to be when you grew up?
I always dreamed of working in the film industry, whether as an actor or behind the scenes as a producer, director, or editor. I even earned my Bachelor of Business Administration (BBA) with a concentration in Interdisciplinary Film and Digital Media from the University of New Mexico (UNM), where I explored both business and film/video game production. I later went on to get my Master of Business Administration (MBA) from UNM with a dual concentration in marketing and operations.
Marketing turned out to be a great fit because I get to blend creativity and strategy—sometimes even producing videos!
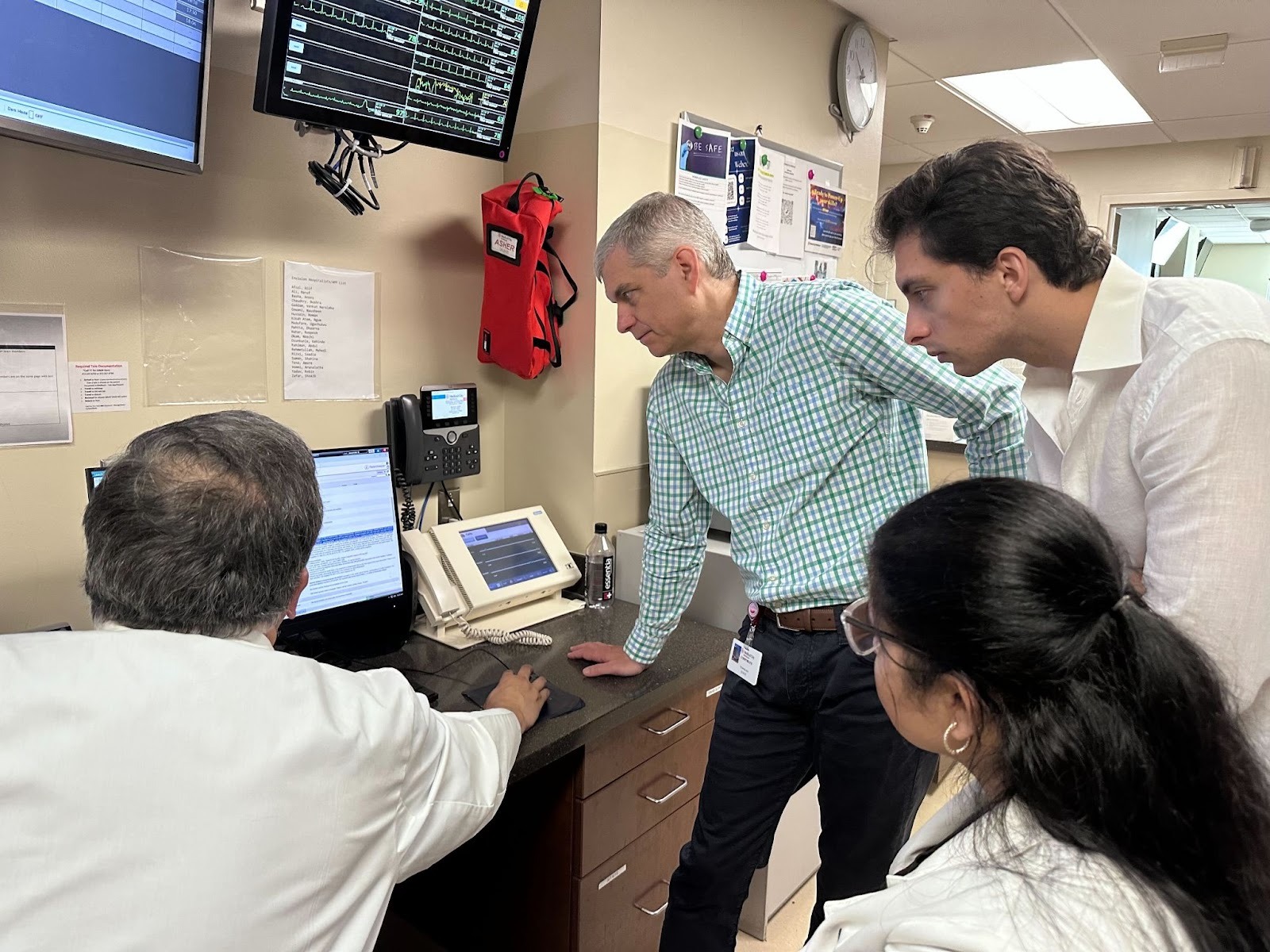
Describe a day in the life of your role.
No two days are the same in marketing, and that’s exactly why I love it! There are so many different facets to marketing. One day, I might be deep in analytics, reviewing campaign performance and building reports to improve our marketing strategy and tactics. The next day, I might be storyboarding an explainer video or planning an industry event. I also work closely with reporters and editors to shape narratives on healthcare innovation. As marketers, you can easily be someone who is really focused on one specialty, or you can wear multiple hats. I prefer to do it all, and Commure enables me to do that.
What made you decide to join Commure?
I joined Commure through the acquisition of Augmedix, but I had already known of and admired the company. I was at Augmedix for five years prior to the acquisition, and I was the very first marketing hire. I got to build out everything from growth marketing to marketing analytics, and got to work with all of our executives, including Ian Shakil, who founded Augmedix and is now the Chief Strategy Officer at Commure. He's a wonderful mentor of mine, and I learned so much from him during my time at Augmedix and am grateful to continue to work with him at Commure.
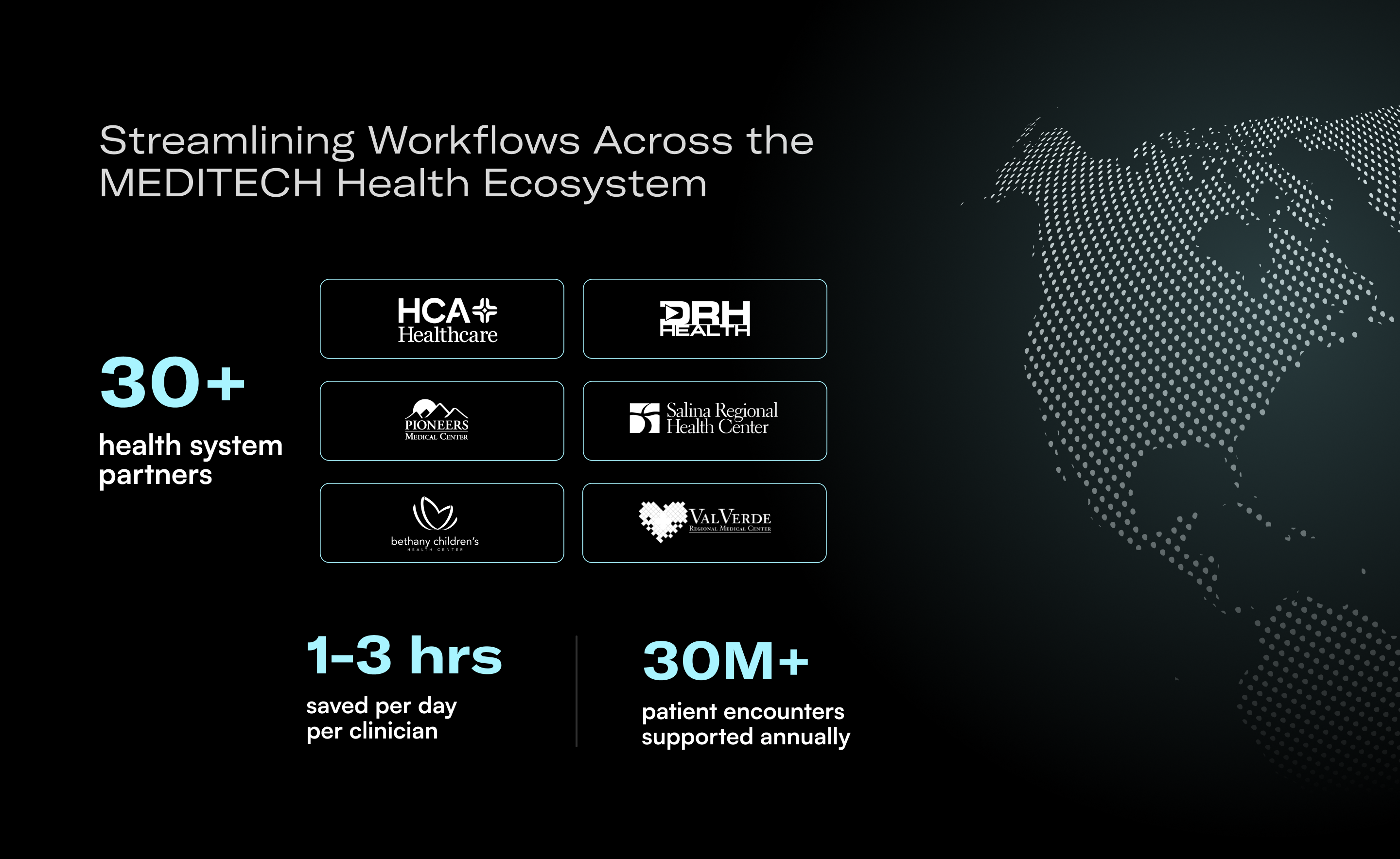
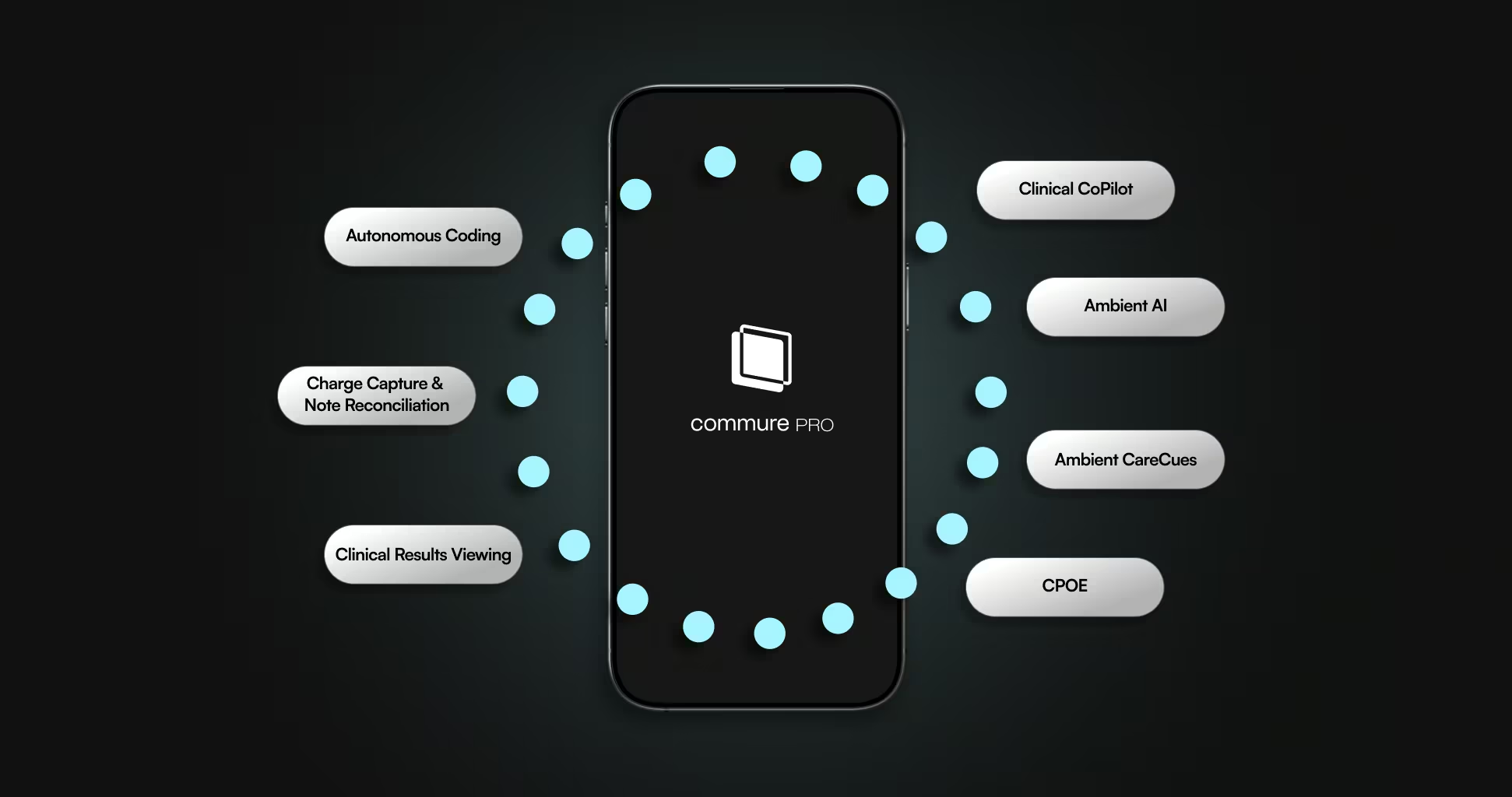
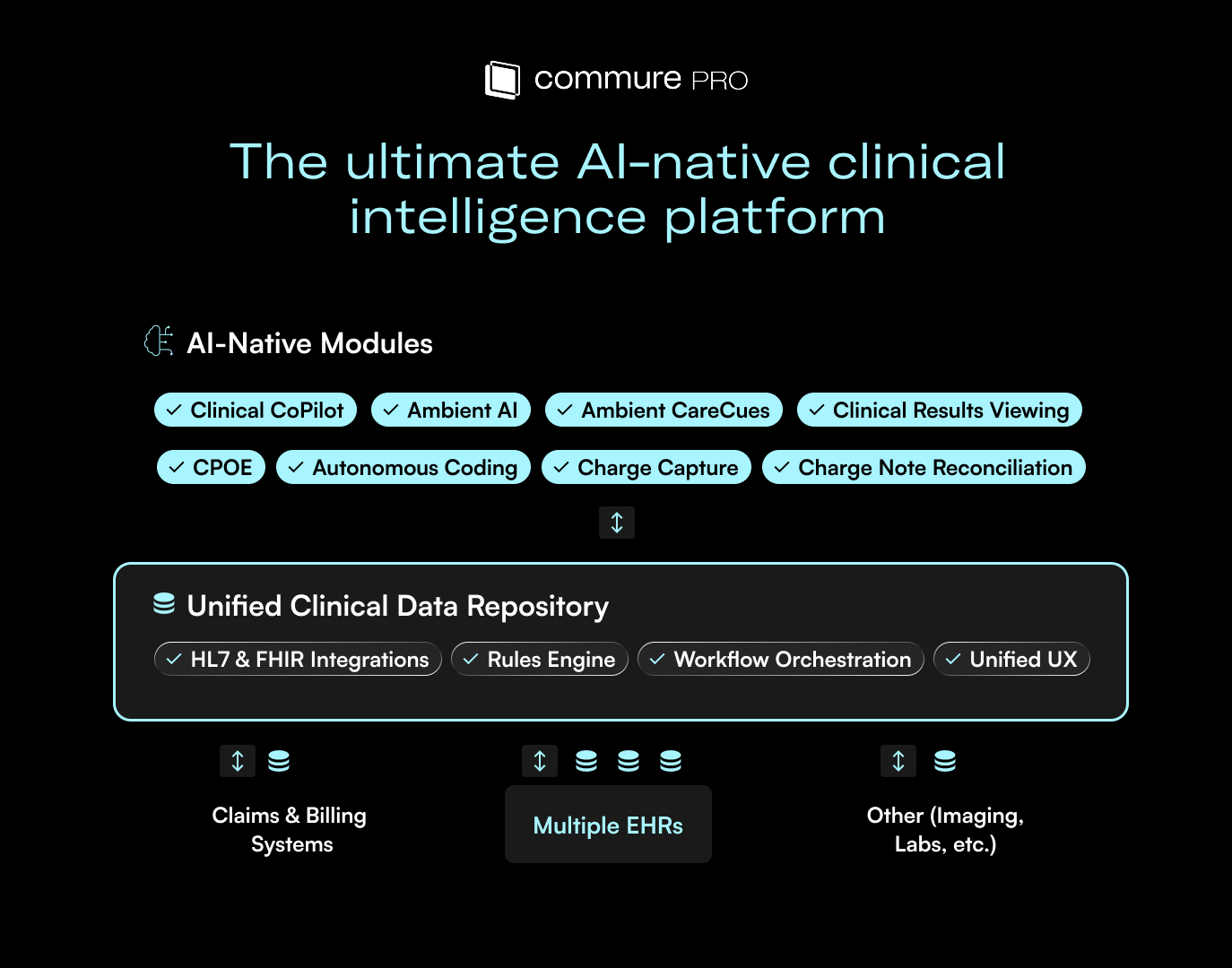
Commure’s mission and platform model (an interconnected suite of AI-powered products built in partnership with leading health systems) really resonates with me. The mission to transform healthcare through cutting-edge technology is something I deeply believe in, and I’m excited to help bring that vision to life through thoughtful, high-impact storytelling and marketing campaigns.
How would you describe the Commure company culture?
Commure has a strong “Day 1” culture where every day is an opportunity to innovate, move quickly, and make a real impact. We act with urgency, take extreme ownership, and focus on delivering meaningful results.
It’s a fast-paced, collaborative environment where high performers thrive. Augmedix was a fast-paced culture as well, and we all wore so many different hats and took so much ownership. Now, as a part of Commure, I love the fact that a lot of the cultural values and work ethic are very similar. Now, it's just a way bigger team!
What advice would you give someone on their first day at Commure?
Be customer-obsessed and prioritize speed. Take time to learn the product suite inside and out, it will help you ramp up quickly and build strong cross-functional relationships to be highly effective. Be curious, be bold, and don’t be afraid to jump in and make things happen.
What are your greatest accomplishments so far at Commure?
I’ve only been at Commure for 8 months, but I’ve made significant progress on our public relations and corporate communications strategy. Specifically, in Q4 2025, Share of Voice (SOV) increased 231% in media mentions since Q3 2025 (when no PR strategy was in place) and 467% in audience reach, outpacing all of our top competitors in audience reach. These SOV results demonstrate the value of proactive media engagement in elevating Commure’s presence.
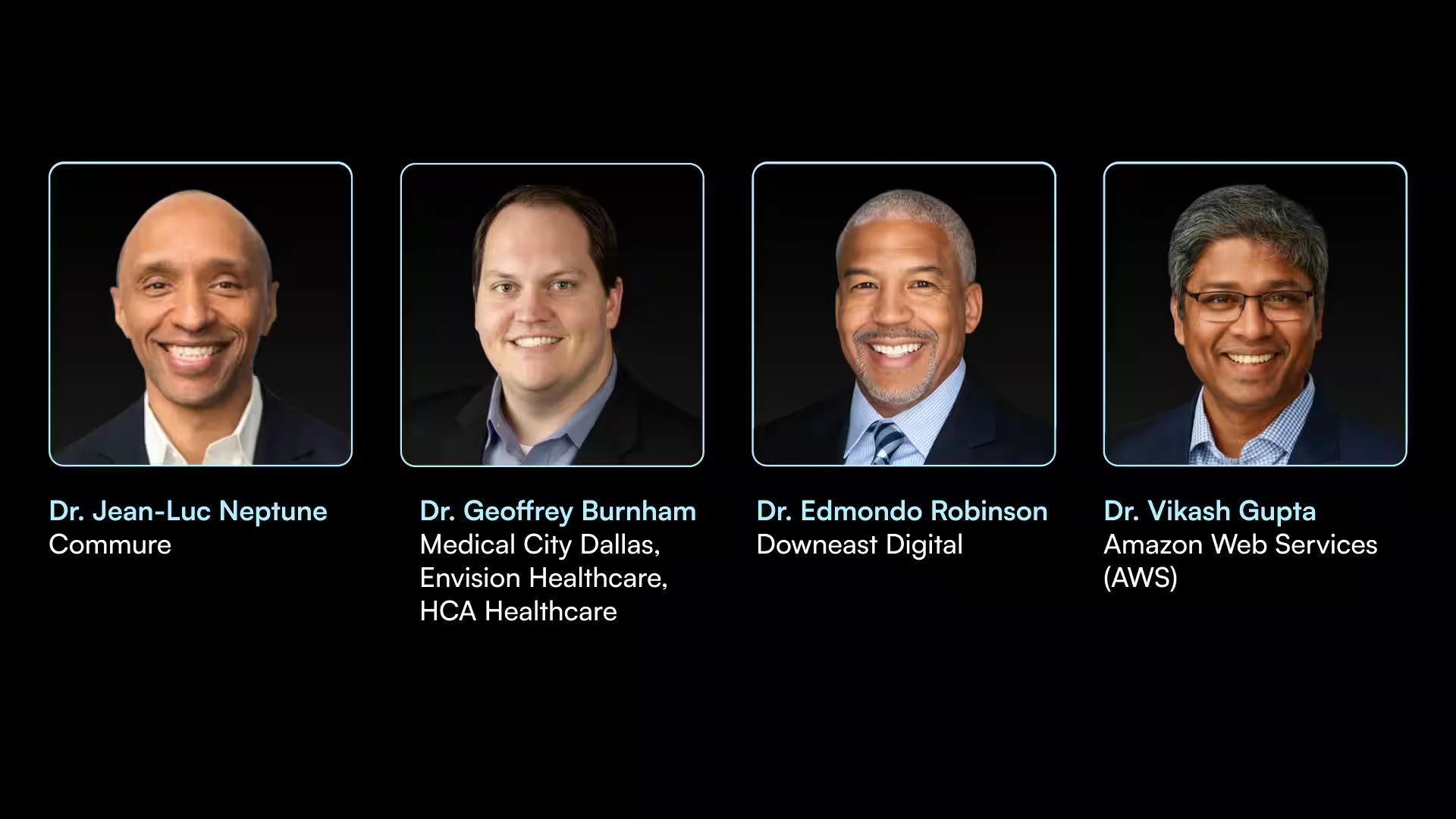
Additionally, in Q2 2026, I helped plan and host the inaugural Commure Nexus event! This executive summit welcomed 40+ healthcare leaders to San Francisco for a day of curated discussions, live demos, and executive keynotes from top voices at Commure, General Catalyst, Amazon Web Services (AWS), and leading health systems. I'm already looking forward to planning the next event and continuing to collaborate with the brilliant minds shaping the future of healthcare.
Interested in a career building the next generation of healthcare technology powered by AI? We are always looking for talented people across our departments.





.avif)

.png)